Evidence based orthodontics is not as straightforward as it seems
Over the last few years my blog has been popular because I publish posts on orthodontic evidence. However, can we really practice evidence based orthodontics?
Recently, I have been in many discussions about the adoption of orthodontic techniques in the absence of evidence. Indeed, we are all aware of the inventors, early adopters, snake oil salesman and other promoters making claims about treatment. This has led me to consider whether we can practice evidence based orthodontics. As a result, I have decided to revisit a post that I did several years ago and see if my opinions have changed.
Should we practice evidence-based orthodontics?
This is a basic point and a good place to start. However, people have pointed to me out that orthodontics is unique because it is an art. Furthermore, any the harms that we may cause are usually minor, for example, decalcification and root resorption. It is, therefore, not necessary for us to practice evidence based care.
I disagree. This is because we need to ensure that our treatment is based on evidence, when it is available. We also need to inform our patients of all the potential risks and benefits of treatment. To this end we should be particularly careful of making statements that are not based on good research evidence. I can think of the following examples, the proposed benefits of non-extraction treatment, methods of speeding up treatment and orthodontics that is provided to reduce sleep disordered breathing in children. It is also important for us to consider that charging patients for these treatments does cause harm to their wallets.
 Where do we get the evidence?
Where do we get the evidence?
It is easy to state that the best source is the scientific literature and we can find an increasing number of published trials and systematic reviews. Nevertheless, the quality of the published papers does vary, even in the refereed literature. As a result, it is essential that we can spend time reading the papers and applying our research knowledge to the findings. Alternatively, we can obtain information from magazines, the internet and even this blog. All provide information of varying quality and perhaps lead to confusion.
When I have looked at recent trials, it is clear that studies are being carried in several important areas, for example, self-ligation, methods of speeding up treatment and temporary anchorage devices. While this is great progress, there is a tendency for investigators to concentrate on treatment mechanics. I have done this in several trials that I have done. We still need to investigate some fundamental questions, for example, to identify the benefits of orthodontic treatment, the effects of orthodontic treatment on the airway and whether we can intercept the development of malocclusion. As a result, there are gaping holes in our knowledge. How do we fill these gaps?
It is not all about evidence!
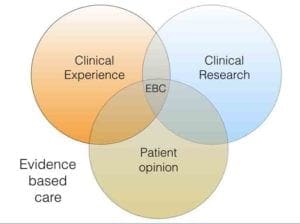 When I look back over the development of evidence based orthodontics I think that one of the problems was that orthodontists “discovered” trials rather late. Several of us became keen to encourage orthodontics to “catch up”. As a result, I put a great deal of emphasis in my writing and presentations on promoting the value of trials. Looking back, I think that I failed to consider that evidence based care is based around a combination of research evidence, patient opinion and clinical knowledge and expertise.
When I look back over the development of evidence based orthodontics I think that one of the problems was that orthodontists “discovered” trials rather late. Several of us became keen to encourage orthodontics to “catch up”. As a result, I put a great deal of emphasis in my writing and presentations on promoting the value of trials. Looking back, I think that I failed to consider that evidence based care is based around a combination of research evidence, patient opinion and clinical knowledge and expertise.
While this concept is now clear to me. I feel that I should point out that this does not mean that these three components are equal. The proportion of each component that influences a final clinical decision is influenced by their relative strengths. For example, there is no doubt that if good scientific evidence is available it should outweigh clinical experience. In fact, we are not practicing ethically if we do not explain the presence or absence of research findings to our patients, so that they can make informed choices about their treatment.
Information we need for patient consent
For example, if we consider the use of TADS. We now have the evidence to say to our patients.
“I would like to use a TAD because it is effective in maintaining anchorage, is easier for you to manage than headgear and it comes with less risks”.
Conversely, if we are proposing that we provide treatment to treat sleep disordered breathing in children, we should be saying
“I would like to propose a treatment that is based on very limited research but my clinical experience suggests that it will help you.”
Importantly, if we are going to take the second approach, we need to justify why our clinical experience is so important in the absence of research. It is also crucial to inform our patients of studies that do not show any benefits for our proposed treatment. Good examples of this are the studies on self-ligation and methods to speed up treatment.
 Where do we get our clinical experience and knowledge?
Where do we get our clinical experience and knowledge?
This now brings us full circle. If this is going to be a crucial part of the decision making process, we need to identify how we gain this information. At the simplest level this is by treating our own patients and discussions with colleagues. But, we need to make sure that we do not only just remember the cases where the treatment “worked”. Our failures are of equal importance. We also need to consider our personal clinical experience and consider whether this is sufficient to base treatment decisions upon.
Other sources are attending conferences, the use of social media and listening to advocates for particular treatments and interventions. Again, we need to be cautious as this information tends to be biased towards the successfully treated case. This is because most speakers show their successes (many times). The other source is the salesman and this is not the best way to obtain information for evidence-based care. Nevertheless, this does influence prescribing!
Summary
I hope that I have managed to outline the issues that we face. My general feeling is that we should base our treatments on the evidence. When it is absent, we need to accept that our treatment is based mostly on clinical experience. We need to explain this to our patients. When we do this we are practicing evidence-based orthodontics.

Emeritus Professor of Orthodontics, University of Manchester, UK.
Well said. Balanced post.
What is certain is that evidence based driven practice is the only way to preserve orthodontists from commercial induced comportment.
Hi Kevin!
I love your Venn diagram, reminds us to consider all 3 factors in providing evidence based care and that the proportions are fluid between patients.
Your conclusion; that generally we should base treatment on evidence seems logical and appealing until I wonder what standard of evidence qualifies for justification of treatment plans? Its been a while since Lysle Johnston announced “let them eat cake”!I I encourage bloggers to follow up this weeks blog by visiting your November 24 2016 blog regarding the hierarchy of evidence and the elusive holy grail of the RCT. VV
Kevin, very nice summary. I often wonder if the EBT zone would dramatically enlarge if all the residency research worldwide was “published” by being electronically available and searchable somehow.
Evidence is important and generally we should treat patients accordingly. but when Invisalign used to advise on 14 days aligners change
Patients who used acceladent could sometimes change in seven days. Now we know that perhaps it wasn’t due to acceladent but due to Invisalign as that we know we can change aligners after seven days, many times. However at that time patients who spent more money and wanted to shorten their treatment did receive what they wanted and if they haven’t paid they would have a much longer treatment. This example shows that if patients and professionals follow only the existing evidence then in this particular case the treatment would be twice longer. I trust you understand the point I wanted to say
Thank you Kevin – I couldn’t agree more on what EBD & EBM is wrt 3 main components.
As you know I have been pointing this out for some time, with great resistance initially but less so now.
Of course we will no doubt have further discussions about the proportionality and influence of each of those 3 key components 🙂
Again thank you for highlighting that EBD and EBM isn’t as straight forward as knowing the literature alone and until it is robust in all aspects, realistically, I suspect that published evidence will only have ‘low’ confidence for dependency upon EBD decisions for the majority of clinical cases we treat every day.
In truth this is so for my Speciality of Prosthodontics too, a sometimes bitter pill to swallow, I acknowledge.
Yours also realistically,
Tony.
dear Kevin,
I have followed your posts with much interest hoping that you might eventually look at our specialty from an outsider’s viewpoint. I have attached a link to a recent article, peer reviewed., which suggests that we are a long way from developing the possibilities. In fact we have to start over at the kindergarden level. The link is oral health archives march 2018. My web site is http://www.orthodonticed.com. Our specialty has the tsunami of Invisalign coming down on it. If we can’t do better than our current performance we deserve to be swept away.
. Read the article . What is going on is fascinating and quite accessible to investigation.
After more than 60 years in orthodontics there has never been a better chance for our specialty to become a true health service but not with the present outdated paradigm.
Gavin James
BDS MDS FDS ( Eng ) D Orthodont. ( Tor)
Kevin, thank you for an excellent and timely article on a topic that I am sure many of us are very concerned about in treating our patients as well as we can.
Hi Kevin:
I am confused by your summary statement, “When it is absent, we need to accept that our treatment is based mostly on clinical experience. We need to explain this to our patients. When we do this we are practicing evidence-based orthodontics.” Is there a typo here? It reads as if you’re saying that if there’s no evidence, treatment will be based on clinical experience instead. If that is the case, then Dr Snakeoil says to his patient, “There’s no evidence for my snakeoil protocol, but my snakeoil treatment option is based on my clinical experience since I’ve used it successfully in the past on other patients”. Here, Dr Snakeoil presents the risks, benefits and alternatives to his potential patient and – on obtaining informed consent – might proceed with his snakeoil therapy. So, is all evidence equal – but some evidence is more equal than others? Maybe I’m missing something??
when reading systemic reviews and meta analysis articles on any topic they usually end up with 1-2 acceptable articles
this is quite discouraging because I feel that alot of those rejected articles have useful information but unfortunately bad research design thus leading to their disqualification
Morning,
It’s just amazing how much over-complex magical thinking there is in Ortho. I’m not sure that other branches of dentistry (other than possibly TMD and occlusion) have the same bewildering variety of opinion. In addition, what evidence we have gets ignored. It strikes me that we have 3 good pieces of evidence 1: Aligning teeth has no health benefit (Shaw) 2: Teeth move as you get older especially lowers (Little): We cannot grow jaws (your good self et al) and yet these are regularly ignored. Teeth are not bothered if straight or crooked they just want to fit as best as possible, bearing in mind the shape of the face, and this fit will inevitably change as we grow and our faces change. We have phases of growth and things can change quicker during these periods. In a nut shell. I’m not sure it’s more complicated than that.
Hi Andy- Thanks for your comments on EBC. I disagree (partially) with your statement that “aligning teeth has no health benefit.” One of the problems with clinically based research where we throw hundreds, sometimes thousands of patients into a pot and do some fancy statistics on them, is that each person’s situation is unique. I could show you hundreds of situations where crooked teeth caused major issues. The easiest one might be a partially erupted 3rd molar that is mesially inclined resulting in zero chance of cleansing. The patient wakes up with a swollen jaw and severe pain. Death is a possibility if untreated. So, we have to be very careful about making blanket statements in the literature or in our interpretation of it. Common sense must prevail. Please do not take this statement to the extreme limits of 1 mm of lower arch crowding is bad for you. That’s not what I’m saying. “Health benefit” is a pretty broad term. Are we considering mental health for example? Gingival health? Where do we begin…
I thetr a place for evidence based meficine or is it a form of popularistic medicine.
Each person suffering becones a patient.
He is an Individual that comes to a specific medical prsctitioner and entrusts him to trrat his condition.
His condition based on Psyco Social Bio thinking is specific to this individual patient.
Why base our treatment on what works or what is poular or what is financial better or what pharmaceutical companies are pushing.
Could all this evidence based result not be applicable to our patient
Do we not need to treat our patient
What I like about the process you follow to make a final decision, is that you end up relying on ethics! Thank you for rising the awareness in this matter.
Good morning Professor,
what do you think about a Practice Based Orthodontic Network or an Orthodontic Registry to solve the problem?
Could be clinical epidemiology the right answer ?
Thank you for your exciting blog
Alberto
what do you think about a practice-based orthodontic research network or an orthodontic registry?
Very sound article and much appreciated.
Dont make the mistake in presuming that things are different in life threatening areas of medicine —they are not!
Clinical practice is an amalgam of many issues !