A simple summary of the need for Orthodontic Extractions..
Orthodontic Extractions: a simple summary
This is Billy Biley, a cartoon character drawn by my son when he was seven years old. There may be a deeper meaning to this picture, but it now reflects my panic since I opened the Pandora’s box of orthodontic extractions.
In my previous three posts, I outlined research projects that evaluated the effects of orthodontic extractions on soft tissue profiles and obstructive sleep apnoea. These studies have used several research methods, for example, retrospective analysis, evaluation of “big data” and a systematic review. They have all concluded that extractions did not have a “harmful” effect. But what do I really think?
Evidence-based dentistry
Whenever we take a clinical decision there is always uncertainty and the role of research is to help reduce uncertainty (see this post). It, therefore, follows that the higher the level of evidence the less clinical uncertainty.
Regular readers will be familiar with the pyramid of evidence and when we apply this to the studies that have been carried out, the level of evidence may be considered not to be high. But does this mean we cannot practice evidence based care when we are faced with the decision to extract or not?
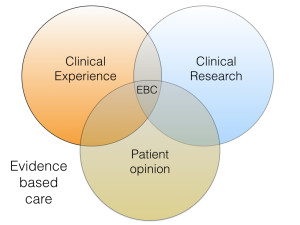 If we only looked at the research evidence this would be the case. Fortunately, evidence-based care is not only based on research but is based on a combination of evidence, clinical experience and patient preference.
If we only looked at the research evidence this would be the case. Fortunately, evidence-based care is not only based on research but is based on a combination of evidence, clinical experience and patient preference.
So how do I decide?
The most important point that I would like to make is that I do not like recommending orthodontic extractions, they are traumatic to patient and my mechanics are more difficult. I take this decision by using the evidence based care process that I described. Firstly, it is clear to me that there is often no need to extract teeth when there is no crowding. Furthermore, if an overjet is increased I will not extract to retract the upper incisors. I will use a functional appliance that would retract the upper and proline the lower incisors (perhaps creating another problem!).
If there is severe crowding, I am more likely to extract, as in my clinical experience this is the only way to make space. You will note that I will not be developing the arches with special brackets, remarkable removable appliances or myofunctional appliances. This is because there is minimal evidence that these are effective. I also know that I cannot move upper molars more than an average of 2 mm distally. As a result, I feel that the only controversial area on the extraction decision is when there is moderate crowding. It is also important to consider that the decision to extract should not be considered in isolation. I cannot help feeling that “over retraction” of the upper incisors is not the result of the decision to extract, but is mostly influenced by the choice of treatment mechanics. I am, therefore, confident that the profile is unlikely to be unduly influenced, for Class I skeletal patients, if I extract and use correct mechanics.
I also know that relapse is unpredictable and I cannot guarantee to my patients that their treatment will not relapse.
Finally, I think that by now I am a competent orthodontist and I can treat extraction or non-extraction equally well.
As a result of this process, the person who has the final say is my patient. I simply present the the points above and let them decide. It is no surprise that most of them do not want orthodontic extractions and so I tend to treat more moderate crowding cases without extractions. From discussions with colleagues this appears to reflect contemporary orthodontic practice
Why the new controversy?
Orthodontists have been debating the need for extractions for many years. From time to time we think we have an answer. But every now and then the flames are fanned and we start arguing again. This seems to be happening at present and I would like to give my personal opinion on the reasons for this.
I cannot help thinking feel that the people who promote “new” orthodontic techniques and philosophies to general practitioners on short courses, with the aim of getting them to use their appliances are responsible. This is because is also not possible to treat extraction treatment mechanics on a 2 day course. As a result, the people promoting the new developments promote a non-extraction philosophy based on the premise of arch development (expansion).
They also paint a picture of orthodontists being old-fashioned, out of touch and protectionist and the non-extraction/extraction wheel keeps turning…….
I also have come across advertising in the UK that suggests a child can have orthodontic treatment, at no cost on the National Health Service, and they will have to have extractions. But if they wanted their arches “developed” with special brackets or removable appliances then this treatment could be provided but only on a private funding basis. So, this is a serious issue.
In the comments section of my last post people pointed out that studies into extraction/non-extraction do not measure the airway or use 3D measurement. I would hope that if these studies are repeated they could be done prospectively and this would give investigators the opportunity to use contemporary techniques, but there is also a danger of looking for something that is not a problem. Furthermore, it is easy to criticise studies that have been done many years ago. Importantly, I am still to see the evidence for the effectiveness of myofunctional therapy, breathing exercise and influence of airway volume. I may have missed it, so if you are reading this and are aware of any work in this area, can you let me have the references and I will continue the discussion.
Finally, I would like to point out that some readers may think that my interpretation is too simple and I expect that there will be some comments on this post. But remember, if you are going to make claims for certain treatments, philosophies and miracles could you provide some proof?

Emeritus Professor of Orthodontics, University of Manchester, UK.
What about the evidence supporting functional orthodontics + palatal expansion (even in adults) found from the work of Docs including but not limited to: Bill Hang (California); Kevin Boyd (Chicago); Derek Maloney (Australia); John & Mike Mew (London)-just to name a few? The issue of funding should not trump what is best for patient outcomes. How can the contributions of extractions to airway collapse (among other issues) be ignored? Not sure why you bring up the funding issue. In U.S, dental and ortho insurance coverage is rarely, if ever, covered in full even for peds and certainly not in adults.
My search of PubMed did not reveal any “contributions of extractions to airway collapse (among other issues) “. None of the studies in PubMed that cite change in “airway space” actually look at this relationship to sleep apnea via a sleep study (PSG). As a matter of fact, the only scientific study that analyzed premolar extractions and their relationship to Obstructive Sleep Apnea found that there was no relationship:
“Evidence Supports No Relationship between Obstructive Sleep Apnea and Premolar Extraction: An Electronic Health Records Review.
Larsen AJ1, Rindal DB2, Hatch JP1, Kane S2, Asche SE2, Carvalho C3, Rugh J
J Clin Sleep Med. 2015 Dec 15;11(12):1443-8. doi: 10.5664/jcsm.5284.
Hi Ann, thanks for the comments, I reviewed this paper a couple of weeks ago on this blog. Are you the first author?
Yes, I am the first author. Thank you for your nice review.
What research? Where can one locate this evidence on airway collapse and these other claims which border on pseudoscience? Please post citations. I suspect there is no reliable, quality evidence since several of these claims have been disproven in the scientific literature.
Dear Kevin,
I find myself strangly torn, because I agree with some of your points, but not others.
So let’s start with some agreements – the highest levels of clinically trialled evidence would be ideal for all or much of what we do, but frankly it isn’t and in Ortho. Particularly, there is LOTS of published research proving absolutely nothing !!!
Example – Cochrane review ( highest level we have?) of class 2 cases says one cannot prove ANY benefit of ANY Orthodontic intervention THUS doing nothing is evidently as good. NOTHING !!!
So I agree some published evidence is nice to have, but in evidence-based care the other 2 circles are ‘clinical experience/opinion and Patient choice!
Clearly with a LACK of conclusive evidence-base throughout ALL of Orthodontics, those two other circles become more significant overall !!!
This we agree (I hope) that published evidence is desirable but apart from a couple of rare instances (eg: Trauma reduction for 9mm+ OJs) there is no, repeat NO evidence Orthodontics improves health. NON, because Orthodontics is about 99% cosmetic in nature 😮
Personally I still believe that to be a very valuable aspect socially BUT let’s just stick to published conclusive evidence for now and be willing to admit, there isn’t any for 99% of what we do 😮
Thus I say this with the greatest respect Kevin, your blog starts off quoting Evidence-based care and that 3 circle model for ‘Optimum’ provision on an individual basis (excellent IMHO) but then rapidly deteriorates into an ”Opinion-based” descriptor of what you think other people do or don’t do, either as Specialists in Hospital or in Practice or so-called ‘weekend’ courses as if they are indesputable fact.
They are of course ‘opinion’ only and maybe based upon some isolated examples you’ve heard or seen for yourself, but hardly a ‘representative sample’ or with a control group, is it ???
Now it is your blog and blogs are about opinions too and it is entirely right you express those without fear or favour – it is in your name afterall 🙂
But some do have differing opinions OR experiences OR observations too, which are equally valid or worthy of consideration, ESPECIALLY within the 3 overlapping circles of Optimum care for each patient.
I’m sorry I’m writing this upon my phone and it’s gone on longer than I intended, but I cannot sign off without mentioning ‘moderately crowded’ cases and extractions.
I am pleased YOU do a lot less extractions now and of course what dies ‘moderate’ mean and is there a mild-moderate or upper-moderate scale, but if you read any contemporary Orthodontic textbook, the MAJORITY either directly or indirectly assume/exemplify Extractions will be prescribed in ‘Moderately Crowded’ cases !!!
They most certainly do NOT give the impression of the very clear ‘dilemma’ or ‘angst’ approach you have described in your blog, today and previously, about whether to extract, or not, in moderately crowded cases of any type.
Actually I shall end there, on something we maybe agree upon more than disagree upon.
Yours observationally,
Tony.
It would be interesting to know what our Periodontal colleagues have to say on the potential long term implications for periodontal health due to extraction/non-extraction orthodontic treatment…
I second this suggestion
I think the difficulty is in agreeing a definition of “moderate crowding.” To some extent, it depends on what you believe the correct archform for a patient to be.
For what I’d see as “moderate crowding” in an arch that didn’t have lingually/palatally tipped teeth, my preference would be towards space creation (IPR/distalisation/extractions) for reasons to do with long term (50+ years) periodontal health.
I don’t know what’s going to happen in that time. I do know that widening the arch with fixed appliance generally reduces the volume of alveolar bone buccally. I am assuming that in the long term that will not be a good thing. I have no evidence to argue that point either way .
That’s what I’d tell a patient if the asked.
Disclaimer: I am only able to read the abstract. Would you have the opportunity to review this research from 1997 on myofunctional therapy and the reported benefits to occlusion? Thank you
http://www.ncbi.nlm.nih.gov/m/pubmed/9487828
Here are 2 good reference for myofunctional therapy and orthodontic treatment:
1. Dr. William R. Proffit on the proper role of myofunctional therapy.
Proffit WR, Brandt S.
J Clin Orthod. 1977 Feb;11(2):101-5. No abstract available.
PMID: 273603
Similar articles
Select item 1053783
2.
Myofunctional therapy for tongue-thrusting: background and recommendations.
Proffit WR, Mason RM.
J Am Dent Assoc. 1975 Feb;90(2):403-11. No abstract available.
PMID: 1053783
Similar articles
you might want to contact her directly [email protected]…..she is an excellent OMT judging from the results I have seen over the past several years.
I’m not Dr. O’Brien, but the paper by Benkert defies classification as a scientific paper (based on the abstract). There is no mention of type of study, sample size, selection criteria etc. And they have no control group owing to “ethical conflicts” – how convenient. It is significantly flawed pseudo-science like this that make it impossible to every verify any claims made by the proponents of fringe therapies.
You talk about the debate on the need of extractions. In my lay opinion (although I am a previous orthodontic patient) I would say the real debate is why malocclusion is occurring at all. Could I ask for your opinion on mouth breathing as a causal factor (and other commonly sited factors such as soft foods and NNSH) in the development of malocclusion? From my brisk search of this website it seems to have been given only scant attention.
Missing teeth and pediatric obstructive sleep apnea.
Guilleminault C1, Abad VC, Chiu HY, Peters B, Quo S.
osama alsaddik Thank you for replying with that article. I would be inclined to say that the causes have been understood for a long time before last year. Do you think it is a fair assumption that it has simply been ignored in the dental profession?
what about the need of compensating extraction in a situation where the lower first permanent molars are missing on class I skeletal base/ permanent dentition ? ?
Dear Prof O’Brien
Per your “….In the comments section of my last post people pointed out that studies into extraction/non-extraction do not measure the airway or use 3D measurement. I would hope that if these studies are repeated they could be done prospectively and this would give investigators the opportunity to use contemporary techniques, but there is also a danger of looking for something that is not a problem. …”
With all due respect Prof, you seem to imply from this statement, and several of your previous postings on this forum, that unless published data is derived from prospective longitudinal, randomized, blinded trial protocols, you will not allow yourself to be curious about existing evidence that might suggest current orthodontic Dx/Tx philosophies might be in need of revision so as to reflect new evidences (e.g., per your Class part 2 posting, the several references RE early expansion/protraction, airway, neurological/neurobehavioral implications, etc. that I’d sent to you last June that you indicated as being ‘inconclusive’ ). Granted, blinded prospective RCT’s are indeed deservedly deemed as the Gold Standard for many/most clinical research endeavors, but please consider, sometimes it is in the best health interests of our young patients, to ‘act’ on the best ‘available’ evidence (from non-RCT’s), rather than it would be to ‘wait’ for the best ‘expected’ evidence (under conditions of RCT design); and furthermore, conducting a prospective trial as you’d suggested, for the purpose of investigating impact of ext vs. non-ext. on 3-D airway, given what we now clearly know about how malocclusion-related pediatric SDB/OSA can impact neurological development, do you really think that you could get this type of protocol approved by your Institutional Review Board (i.e., would you want your young child/grandchild to be in the control cohort?).
Respectfully
Kevin Boyd
I am now interested in what constitutes “moderately crowded” – and then do you allow for other space-demanding aspects of the mechanics like arch levelling – can we have a blog on this topic too? Is there much consistency among clinicians on the topic?