MARPE: Are longer minscrews better?
Our obsession with maxillary expansion continues to apply with many techniques in common usage. These range from removable appliances, which are likely to tip teeth, to fixed appliances, which, depending on their rigidity and rate of activation, may produce either dento-alveolar or combined skeletal and dental effects. There is, of course, lots of ongoing discussion around the downstream effects of this expansion. I am unconvinced that expansion does much more than objectively improve transverse relationships and will, therefore, make no promises to patients regarding the associated subjective change.
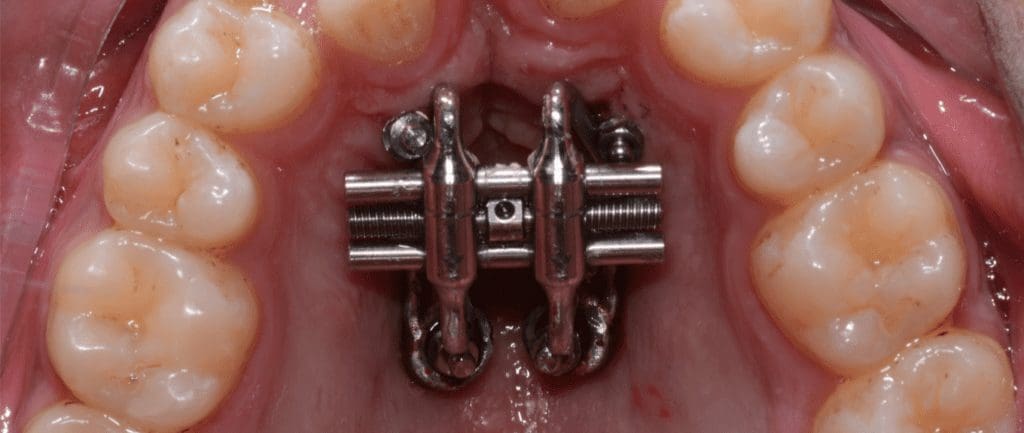
Nevertheless, skeletal expansion can be beneficial in addressing transverse issues in certain patients. The selective use of MARPE may help to prevent the need for more invasive surgery in skeletally mature patients. Longer miniscrews can obtain bicortical engagement of the palatal and nasal cortical plates. This has been recommended to increase the skeletal effects of the treatment. There are, of course, risks associated with this more positive approach. We also don’t yet know whether long screws do, in fact, produce a more favourable ratio of skeletal to dental change. The authors of this trial done in South Korea aimed to address this gap in our knowledge in this paper published in the Angle Orthodontist.
Choi EA, Lee KJ, Choi SH, Jung HD, Ahn HJ, Deguchi T, Cha JY.
Angle Orthod. 2023 Jul 1;93(4):390-397. doi: 10.2319/072322-512.1.
What did they do?
They conducted a parallel-group randomised controlled trial. They calculated the sample size and randomly allocated participants, concealing allocation using an opaque sealed envelope system. The operator was not blinded to group allocation; however, the outcome evaluator was kept blind.
Participants:
All participants had a baseline CBCT and had maxillary constriction. They were 19 years and above and had all permanent teeth present.
Interventions:
All patients were treated with the MARPE involving four 1.5-mm paramedian miniscrews. Participants in the control group had 8mm and 6mm anterior and posterior TADs, respectively. In the intervention group, the corresponding figures were 13mm and 11mm (5mm longer).
In both groups, activation was performed at a rate of 0.2mm per day, with a peri-apical radiograph taken after 2 weeks to assess midpalatal suture opening. Further activation until the palatal cusps of the maxillary first molar contacted the buccal cusp tips of the mandibular first molar was subsequently performed. Expanders were maintained for 3 months following active expansion before removal and a final CBCT scan.
Outcomes:
Ten primary outcomes involving skeletal and dentoalveolar change (6 linear and 4 angular measurements) were obtained. The rate of successful midpalatal suture separation and the stability of the miniscrews at the time of the MARPE removal were considered secondary outcomes.
What did they find?
Overall, 32 participants were included in the study, with one being lost to follow-up. The mean age was approx. 23 years with the majority (61%) being male. The suture failed to split in 25% (4 of 16) in the longer screw group, while only one participant (6.7%) did not split successfully in the control group. The primary outcomes were assessed in the remaining subjects only.
A statistically greater amount of skeletal change was observed based on Interprocessus zygomaticus width in the longer miniscrew group, although the mean difference was only 1 mm. More dental change (1.32mm) was also noted in the intervention group in the canine region. No statistical differences were observed between the groups in relation to the other eight variables.
In terms of success rates, the anterior miniscrews were more predictable. Longer miniscrews were more successful posteriorly (96.9%), with shorter posterior screws having a lower success rate (76.7%; P = .024).
What did I think?
I like this study as it provides us with new and helpful information and addresses a genuine gap in our knowledge. MARPE remains in its relative infancy, and, interestingly, current approaches are defined mainly by ‘expert opinion’. It is great to see an attempt to enhance the evidence base to inform our decision-making.
From a methodological perspective, the study was well-designed, involving random allocation to distinct interventions. This approach is the best way to limit the potential effects of confounding and selection bias. I did note, however, that a much higher proportion of participants with longer implants did not split successfully (up to 25%). These participants were subsequently omitted from the analysis. Had the authors included these participants in an intention-to-treat, any potential benefit of longer implants may have been lost.
The analysis included ten outcome measures. Two of these ten outcomes demonstrated statistical significance. Eight did not. While the authors conclude that ‘MARPE with longer miniscrews can increase the amount of expansion of the maxillary basal bone and canine alveolar bone’, it may also be reasonable to speculate that ‘little effect of screw length on the amount and nature of skeletal and dental expansion with MARPE was observed.’
Finally, the authors did not report any notable complications, although some thickening of the mucous membrane at the nasal floor was noted following penetration. Obtaining patient-centred data concerning subjective experiences associated with using shorter versus longer implants would be interesting. Moreover, the high proportion of participants whose suture did not split favourably is notable. The implications of longer implants on imaging requirements are also worth consideration.
What can we conclude?
Using bicortical engagement involving longer mini-implants may produce a minor increase in the maxillary basal bone relative to shorter implants. Any potential effects will likely be very minor (approx. 1mm). Further research examining the impact of implant site and length on the outcomes and complications of MARPE accounting for patient reports would be of benefit. In short, I remain uncertain that there is strength in miniscrew length.

Professor of Orthodontics, Trinity College Dublin, The University of Dublin, Ireland