Should general dentists provide orthodontic treatment (revisited)?
In this first post of 2018, I am going to discuss whether general dentists should provide orthodontic treatment. I have decided to revisit this because of the recent advertising campaigns run by some of the specialist societies, in which they highlight the differences between a specialist and a general dentist.
The first point that I would like to consider is that a general dental practitioner can provide any treatment in which they are competent. This includes orthodontics. Importantly, the practitioner decides whether they are competent and the treatment is within their scope of practice.
While this concept is widely accepted, it is influenced by the aims of undergraduate programmes. These vary throughout the world. In the UK , current guidelines suggest that the newly qualified dentist should be competent in diagnosis and know when to refer their patients to a specialist. The Dental Schools do not train student dentists to be competent in providing active orthodontics.
This raises a problem. If a practitioner wants to provide simple orthodontic treatment and does not want to train to become a specialist, then opportunities are limited. I cannot help feeling that this leaves a “training void”. In some countries practitioners can get experience and attend courses to obtain competence in simple treatment. Some of these programmes appear to be good and specialists run them with high level mentoring. However, others are a greater risk and these tend to be delivered over a weekend. These are widespread and are sometimes run by the “fringe” practitioners. This adds another layer of complexity to this issue.
The counter argument, is that in order for someone to recognise that a treatment is “simple” they need to be fully competent in all aspects of orthodontics. However, it should also be possible for specialists to identify simple cases and provide a treatment plan for the practitioner. Again, in many countries this is standard practice.
Recent advertising campaigns
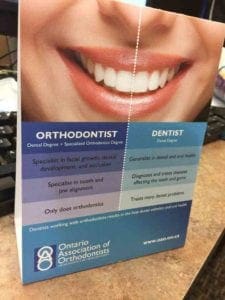
Recently, some of the specialist orthodontic societies have run advertising campaigns to educate the public in the advantages of seeing a specialist. I have inserted two screenshots of advertisements issued by the Ontario Society of Orthodontists and the American Association of Orthodontists.
I thought that the AAO advert was rather controversial and I showed this to some of my general practitioner colleagues. They felt that it was patronising, particularly with the use of the phrases “cleans teeth” and “fixes cavities”. They strongly suggested that if our local specialists put this up in their offices they would stop referring patients.
The Canadian one is less confrontational. Importantly, they point out that generalists and specialists should work together to benefit the patients. I am not sure how effective these campaigns have been, but at least these societies are making an attempt to clarify this issue for our patients. The EOS and WFO are completely silent on this.
The short orthodontic course
I wonder if the target of the specialist society advertising has been the “short orthodontic course”. Subjectively, I feel that there has been an expansion of short 1-2 day courses and “accreditation” in orthodontic techniques. Some educators market “new techniques” that speed up treatment. This is a selling point to the practitioners.
This type of provision also raises the issues of who is responsible if a treatment for a child does not go well? It is clear that this is the providing dentist and not the remote instructor.
I would also point out that specialists do not always provide exemplary treatment. I have made many errors in my career and not all of my treatment has worked well. However, I cannot help feeling that there is less chance of me making a mistake than an inexperienced dentist working to the prescription of a remote prescriber.Importantly, we also need to bear in mind that specialists make unsubstantiated claims on the speed and comfort of treatment, particularly with respect to self ligating systems and accelerated orthodontics using vibratory devices.
Summary
Where does this leave us?
This is a difficult situation and I shall attempt to summarize a few important points
- Practitioners and specialists need to work within their competencies.
- There is likely to be minimal risk from simple alignment of the anterior teeth in adults by a practitioner who is competent.
- Most importantly, practitioners (and specialists) should inform patients of their competencies, their training and experience and be honest about the various systems of delivery.
- We all need to avoid making unsubstantiated claims about our treatment.

Emeritus Professor of Orthodontics, University of Manchester, UK.
In the Netherlands we have also a lot of dental practitioners that are doing orthodontic treatments. This causes in some regions problems with the orthodontists that are critisizing the capabilities of those dental practitioners . Most dental practitioners that are doing orthodontics here have had intensive education and training in orthodontics. In order to differentiate between dental practitioners that are well educated and those that are doing it as “hobby” we have a quality system and register that has the same demands and qualifications as there are for the orthodontists.
To stay in this register you have to qualify every year. This way quality in orthodontics by general practitioners is maintained to the level almost or even equal to orthodontists
What do u think is stopping ur so called well versed gen practitioners from getting university orthodontic program validation… there was a time @ school one could get double promotions HOWEVER the university system works in an entirely different manner.
Great, unbiased commentary on what is still an emotive issue for many in the profession.
I have seen bad work from specialists also. For dentists wanting to specialise, seats are limited to a few per year and also to certain races now due to political decisions. Practitioners Intelligent, capable and reponsible enough should be allowed to practice whether it’s implantology, periodontology or orthodontics. Training is imperative of course
Dear Kevin,
Thank you for stimulating the debate on whether general dentists should be providing orthodontic treatment to their patients or not.
I am a dentist, practising in the rural part of South Africa and my dental practice provides orthodontic treatment to a few hundred patients. I am proud of the outcomes that we have been able to achieve and with the assistance of my specialist colleagues, we have been able to treat some complex cases.
For me, the real issue is about access to healthcare, in this case, orthodontic treatment. The most effective way of increasing access to orthodontic treatment is by training more dentists ( and possibly dental therapists and hygienists) to become competent in the discipline. There will never be enough specialists in the world, let alone in Africa and other under-developed countries to manage all the patients who require orthodontic treatment.
For me therefore, the issue is an ethical and a moral one. We cannot continue to deny billions of people access to healthcare in order to satisfy the professional status and privilege of a few.
Regards
Dr Thabo Twala
Mafikeng, South Africa
I absolutely agree. Teamwork is the answer.. not invalidation and criticism.
This type of internal turf war is not productive ,on many levels ,taking pot shots at colleagues can result in collateral damage ,that is entirely avoidable .General dentists can do whatever falls under a dental license—end of story .Ethical issues are the purview of the individual and the licensing authority.
What would,I suggest ,be more productive,professionally and financially ,would be for GDP,s and specialists to spend their advertising budget on attracting the significant section of the population that does not access orthodontic treatment .
The Canadian orthodontic association was less controversial ? Really ?
https://imgur.com/a/VBvtA
The academy of general dentistry called its lawyers when they learned about the CAO ads, and had them removed.
More to the point, unless you plan to limit the scope of competence of the dentist ( and in this cases complex surgery makes a much better candidates than orthodontics ) the rules stay the same.
The dentist, like any specialist in fact, is the only one who can judge if he/she is competent for doing one particular case. The security of the general public being assured by organisme checking the quality of the work in cases of complaints.
If there are trouble with the quality of care being provided by some practitioner ( I do not specify GP here, because I saw Invisalign treatment done by specialist in Thailand, Singapour, US and Australia which were less than stellar ) , the issue is not better learning but better quality check IMO.
The ad that Kevin refers to is produced by Ontario Association of Orthodontists, not Canadian Association of Orthodontists. They are two different associations.
It comes down to personal ethics. But is your concept of what is ethical Pro-survival for you as well as for your patient?
There is nobody as dangerous as somebody that thinks he knows and doesn’t. This is a universal problem.
Therefor, one should never stop learning and utilize each learning opportunity and never become complacent.
Thank you Kevin.
Again you summarise the issues well. But there is one small flaw. You suggest that all practitioners should be honest about the systems of delivery.
Where money is involved, ethics, honesty and the truth are the first casualties. In my area another specialist offers Invisalign to 8 year olds for the “modest” fee of A$9,000. He also uses Damon and mouth vibrators to reduce treatment time and discomfort.
This makes it difficult to be too critical of orthodentists.
Hi Kevin,
Orthodontics IS Dentistry – it should form a reasonable part of the undergraduate curriculum AND clinical experiences.
I do understand pressures upon undergraduate teachers through budget cuts etc, so clinical experience suffers unduly.
However Orthodontics IS Dentistry (a point worth repeating!) and it should NOT by default, design or monopolisation, become excluded from the GDP range of treatments available to their patients.
Whether it’s Oral Surgery to Restorative, those other Specialists don’t say don’t do a Crown or an Extraction because you are not as well trained as us, they say how can I help you to do MORE work better, certainly the routine treatments, but we are here for you as Specialists for the more challenging or difficult stuff !!!
Imagine if ‘Orthodontics’ behaved like that as a default, by mimicking other dental Specialities……….
Orthodontics IS Dentistry, as are Oral Surgery, Restorative, Endodontics, Paedodontics etc, etc.
Yours proportionately,
Tony.
I write as one who has and continues to teaches my general dental colleagues orthodontics. A few years ago I tried to establish a part-time specialist program to allow experienced general dentists to gain specialist training (and GDC recognition) within the UK, only to be blocked by protectionist orthodontic politics.
The elephant in the ‘UK room’ is the total inability for the UK system to allow experienced dentists being able to either access specialist orthodontic training or being able to undertake an interdependent exam/evaluation (since the Dip in Primary Care Orthodontics was shut down). Hence, a number of independent orthodontic training options have sprung up…….of variable quality. There is a real need to address the desire for dentists to learn orthodontics, this means meaningful engagement by the specailist societies and not protectionism. Specialists cannot argue that general dentists are unable to gain specialist skills without 3 years full time training, yet are happy to work with and train nurses to become orthodontic therapists in 12 months, part-time.
Such have been the developments in orthodontic technology that the technical skills have massively reduced. IT developments means tele-mentoring is now reality. The challenge is to the specialty to stop being protectionist and to engage at all levels, from undergraduate upwards
Declaration of Interest:
I am training director of the IAS Academy and as such I ensure that IAS Academy delivers high quality training, mentoring and patient care. If any Orthodontists doubt this, contact me and i will arrange access to sit in on any IAS training
Isn’t University of Warwick running a part time master programme which on completion could fulfill the requirements for the registration to becoming an specialist orthodontist in UK? There are barrier exams set at different stages of the programmme to ensure the standard of the programme is maintained, not true?
Ross Hobson, I completely agree with you. I wondered if you have a contact email address I could get in touch with you to perhaps discuss this further?
Thanks Kevin,
These areas of scope and competence are changing all through healthcare and need to be discussed.
There are also the meta-trends which are driving this:-
Treatment should be around the patients needs and preferences and accomplishing those rather than our desires.
Referrals increase costs and there is an obligation to the healthcare system and patients to treat at the lowest cost for the best patient assessed outcome.
Ad Hoc CPD is not very effective and we need to find better ways to ensure competency.
In Australia Orthodontic treatment by GP Dentist’s is seeing a significant increase in litigation. There is a concern this is not in fact due to an increase in poor outcomes (though it could be) but perhaps by an increase in the Orthodontists aggressive assessment of those outcomes. Whether this is poor communication by GP Dentists, poor outcomes, poor training or Orthodontists protecting their turf is unknown at this stage.
Ultimately we are seeing the frictions and deficiencies as oral health reintegrates into the broader healthcare landscape and its aims. We now know that this, and the way we integrate evidence about it, will be as much about the internal cultures of the various groups (GPs and Orthodontists).
Trivialising and oversimplified advertising is not helpful, informed debate as you have initiated is.
Paul Beath
I agree, this is an emotive issue for both sides. My concerns as a specialist are the issues around patient consent for treatment. I am extremely respectful to our referring colleagues and agree that simple treatment can be carried out by GDPs if they have undertaken further training and feel it is within their competency. I am just unsure of how consent can be valid if the wider aspects of orthodontic treatment are not wholly recognised/considered and to ensure we do no harm, all risks and benefits must be accounted for before embarking on treatment. I think this is a debate which will be perpetual. I enjoyed this blog post- thank you!
Dear Kevin,
Unfortunately, in my 31 years as a specialist in Orthodontics, I never ever met a simple case. No case is a simple one. You begin with relieving a lower crowding and end up with an open bite. I believe if you hold for a second, you will agree with this statement. Do you really believe that somebody will present his competency to a patient? Do you speak about utopia? I’ll never forget the sentence one of my teacher in the UOP told the current graduates: If you want to succeed be good. no, be better, be the best! Do not devaluate, decrease or diminish the others. Again, be the best. Give your patient the best treatment, time after time. Care for your patient. This is the best way to build a good practice. This is the best campaign that should be recommended. There is no way to fight the general dentists who wants to do orthodontics. This will bring to nothing. I know GP’s that have more than 10 law suits against them and their practice is huge. So…
Be The best you can!
Hi Kevin – Happy New Year to you, family and fellow bloggers!
It is not surprising to me that the orthodontic speciality has attracted disdain and distrust from our dental colleagues. It appears to many that we are aloof, elitist and exclusionary compared to other dental specialists. I experienced this myself as an undergraduate dental student being denied access to orthodontic lectures, yet was welcome and encouraged to attend oral and maxillofacial surgical, pathology and paediatric meetings. Why were these lectures so inaccessible? Many years later, I became Director of Predoctoral Orthodontics at U Pacific in San Francisco. The challenge was immense – to take the lowest scoring course and turn it to the highest and to comply with university accreditation requirements that mandated competency in many aspects of orthodontics for undergraduate students. The issues you raise are not new, not born by systems that purport to make orthodontic treatment simple or automatic, but fertilised by them. I hope that in the interest of patients over the world, especially those in remote communities as pointed out by a fellow blogger, as well as in the interests of the orthodontic speciality we identify cause and definitively seek potential solutions to this historic stand-off.
Potential Cause/s? As the oldest dental speciality; teaching and practice of orthodontics pioneered an individual path rather removed from traditional dental education and practice? Orthodontic treatment plans typically take years to complete and competency is not easily reached within a typical (unmodified) undergraduate dental program? Difficulty in defining and identifying “simple” from “complex” cases? Disagreement on whether “simple” cases, if able to be identified should even be treated by generalists? Self protection of specialist orthodontic organisations and individual orthodontic specialists? Other reasons / combination of the above?
Potential Solutions? Define the objective – we don’t seem to agree even on this. If we do concede as you rightly point out that general dentists may in fact legally practice orthodontics; if we recognise that competency in diagnosis and treatment planning, therefore definition and identification of “simple” cases and treatment of these is required in most undergraduate university curriculum for accreditation of the program – then we are already obligated to carry this educational symbiotic relationship into practice after graduation. There are few examples of this occurring. Continuing education for general dentists run by mainstream speciality with the objectives mandated in the undergrad programs and by law – not just to “baffle them with BS” so that they get scared, learn nothing and are forced into cook book programs run by self-serving entities. Study clubs – on line or face to face run by specialists involving their community of general dentists that lead to more referrals and education of general dentists into current broad literature, diagnosis and treatment planning continued competency as well as treatment of the “simple”/ anterior cases.
If you are an orthodontist reading the above and think that this is unattainable, then you better go and change the dental licencing laws and university accreditation requirements as fist port of call, prior to other current absurd solutions being considered by respected professional organisations such as excommunicating or punishing members who teach and run educational courses to general dentists…..whatever happened to our obligation as specialists to educate and assist patient care? We need to take a look at our specialist colleagues – yes, ortho is different in many aspects, currently however orthodontists are dentists, there is 1 licence, 1 profession and we are part of it until we get so self serving that we dissolve the first dental speciality ourselves, blaming general dentists, orthodontic appliance companies as we fall.
VV
To allign teeth is not a treatment, in the meaning of a clear alligner can do it, by expansion and protrusion. To DO a treatment is an Orthodontist Job.
I am a Senior lecturer for Progressive Orthodontics (POS) in Australasia. The company is one of the biggest teaches of Orthodontics to General Dentists in the World. It is a 18 mths course with many continuing education courses after the main series and an annual Update.
This discussion I have been having for many years. Many Orthodontists are trying very hard to protect their turf. I have no issues with the advertising saying that an Orthodontist is better. Sounds strange to the public,but they can do what they want. Many Orthodontists are sending GP dentists to Dental Boards for no reason to try to stop GPs doing orthodontics. I think this will plan will back fire as GPS see a lot of bad orthodontics from Specialists so will start to do the same thing.
Had a meeting with the ADA and the ASO in Australia and highlighted this point. Our insurances are going to get very annoyed.
But I would like to highlight another approach. One that is a great winner for all. Including the public.
POS will always teach that the GP needs to work with a specialist. No different to those who do endos have an Endodontist on their team. Oral Surgeons and Periodontists etc should be on the team for all GPs. So no different for ortho. But who does a GP send to. Orthodontist cant agree on treatment. Some are Invisalign only. Some dont do phase 1. Some dont do extractions. Some use to say they are a Damon practice. So finding an Orthodontist that you agree with is difficult.
But we still teach to find an Orthodontist who is friendly and who has a similar philosophy.
If there is a class of 50 dentists, 5 will never refer again, the middle group will still refer anything that is more difficult, and the last 10% will refer everything. So wouldn’t you want to work with a GP who is diagnosing better, seeing more ortho, diagnosing what is hard and easy, so learning to refer when beyond their scope and skill and personality level. So lets hope the Orthondontists think of this approach. Make GPs your friend. Spoil us like the good old days. And you may get more referrals. The pie is actually getting bigger.so their is plenty to share. The Smart Specialists will start to work more with the GPs. The archaic ones will start to embarrass themselves and find that GPs stop referring as they are too scared to approach them.
! Right !
The problem isn’t so much the actual provision of care as much as the pseudo-scientific underpinnings behind the fervent beliefs held by several practitioners. This in turn leads to routine delusional claims, misdiagnosis, poor outcomes etc. As a case in point, we see all too frequently these nonsensical claims of extractions ruining faces, causing TMD/OSA etc. And, of course, their “therapy de jour” prevents all these horrendomas. Many of these so-called therapies are divorced from reality with poor to no evidence supporting it. Dental school does a poor job of inculcating critical-thinking skills and those cannot be acquired over a weekend. If practitioners want to provide ortho, then it is incumbent on them to provide it at the level of the specialist. Indulging in chimerical science will only earn the ire of the specialty.
I think that many American dentists are susceptible to “the pseudo-scientific underpinnings” because so little training is given to them as dental students for the treatment of malocclusion, a chronic disorder that, depending on the study parameters, affects 60 to 70% of the American population. The predoctoral dental student should be given training preparing them as competent primary care practitioners in orthodontic therapy similar to the skill level that they receive in the other dental disciplines.
As it stands today, the American dental schools produce only secondary and tertiary care providers to treat a condition that affects the majority of the American population. This is completely contrary to proper population disease management and is the only specialty in dentistry or medicine to do this. I suggest you ask any physicians that you know, especially those in primary care, what they think of this failure and resulting treatment “arrangement”. Watch their body language and, in some instances, you better have thick skin because you may get an answer that may be a bit harsh. Subsequently the void created by American organized dentistry’s failure to educate has been and will be filled by for-profit commercial organizations much to the chagrin of said organized dentistry.
Finally how does this failure to educate serve the public good? How can this be defended?
I couldn’t have agree with you more Dr. Winnick.
POS is 18mths.. trying very hard to teach as much as possible on diagnosing.. The weekend courses are run by Orthodontic Specialists. More money on the courses to be made than in their own clinics?? But the specialty is actually doing the worst training to GP orthos. In Australia, we have to now pay a premium on our insurances to do ortho if you are a GP.. And the major reason is the weekend courses run by the specialists are not training the dentists. I think Vicki put it all very nicely above.
Well said!
Hi Kevin
I was thrown off a very popular orthodontic Facebook group for expressing an opinion on this very topic, perhaps I could have done it better, however isolating and ignoring the conversation does nothing to advance a common goal of “what’s best for the patient”.
One of my new options for treatment has become ‘get a second opinion’ and I document it in my correspondence with my patients. So far 80% of private new patients return for treatment, it went up from 50%. This I hope is another step forward towards ‘ethical selling’ in my humble opinion.
You raise a very important question regarding informing patients of our competencies; is the profession being transparent? I think if we ask ourselves honestly some of else would feel uncomfortable.
The ethical alarm bells are warning enough that one might not be able to stand up in front of the GDC.
I love this thread Kevin, keep it coming, you constantly challenge my thoughts, views and ultimately make me think about my clinical practice.
That sounds like a great idea, IF, dental school were to be 7 years instead of 4. In the four years, students barely have time to gain basic skills and fulfill requirements in restorative, perio and endo. What should we sacrifice to incorporate ortho? Most of dentistry is pathology driven; however, malocclusion is not a disease. This is a different specialty – the diagnostic, treatment planning and biomechanical components require a lot of time and thought to understand (and are a significant deviation from the rest of the DS curriculum). To boot, most cases take 18-24 months of treatment to finish to a reasonable standard. As most who have actually been through orthodontic residency programs will attest, it takes 2-3 years to gain some basic competency. These illusory “solutions” provided by the benighted are completely unrealistic and impractical.
Dear Dr. Ulfr,
“Malocclusion is not a disease” is incorrect. I have included a link (no paywall) to the December 2017 AJO-DO under “Malocclusion and Healthcare.”
http://dx.doi.org/10.1016/j.ajodo.2017.09.005
Point of information: if your country is still using ICD-9, then the code for malocclusion would fall under Diseases of oral cavity, salivary glands, and jaws (520-529) with malocclusion 524.4. ICD 10 has many more codes covering more diseases and comorbid conditions resulting in more precise diagnosis and classification.
Regarding the education of the predoctoral dental students, incorporating orthodontic education into their curriculum is an operations/management issue. I have some ideas about how to do this but I am certainly not an expert in curriculum development but am fairly confident that there are educational consulting firms, at least in the United States, that could aid in implementing a progressive curriculum. I don’t have complete data on this but I think that most recent graduates of American dental schools complete a minimum one-year hospital residency program. If so, then the emerging dentist is effectively trained for five years.
I don’t know if anyone reading this blog has ever experienced this but patients or parents many times will contact their primary care dentist after a consultation with an orthodontist especially if the treatment proposed involves extracting four virgin teeth. Would your practice life be just a little easier if the primary care dentist told the prospective patient the following? “Oh yes, I understand that you’re concerned about removing these teeth but I reviewed Dr. Ulfr’s recommendations and I agree with them. Essentially Andrea has five quarts of teeth in a four quart mouth and if WE want to get a good long time result for her, the teeth need to be removed. In fact, if it was my daughter Maren that had the same situation, I would feel the same way.” Now let’s take a look at second possible conversation. “Oh yes, I reviewed the recommendations and I can see that you’re concerned about removing these teeth. It does seem that orthodontists frequently remove perfectly healthy teeth and I have to admit that sometimes I am not comfortable about them doing this. I am not sure why this done so frequently but maybe Andrea should get another opinion. I have heard that patients sometimes develop other problems having their teeth removed for orthodontics.”
Don’t you think it would be a lot better to go from “I am not sure why they extract healthy teeth so frequently” to “I know that there are situations that this needs to be done selectively”. “I also know that you have heard about problems having teeth removed because of orthodontics but that has been debunked scientifically; it is not true.” Perhaps a little more education would help everybody???
That concludes a couple of thoughts on a Saturday when it’s too damn cold to ski even for a former national ski patroller (and we know how to stay warm) and to make matters worse, the snow conditions are fabulous!
Dear. Dr. Winnick – The link you sent is a letter you wrote to the AJO. Personal opinions of this sort are hardly compelling evidence of the fact that malocclusion is not a disease. What, in your opinion, is the consequence of not treating this “disease”. As someone involved in education on both the dental and ortho sides, the skill set needed is significantly different – a lot more cognitive and reasoning skills are required for orthodontics. The paradoxical fact is that, unfortunately (based on my observations/experience) the vast majority of dental students seem to find ortho mind-numbingly boring when it comes to the theory/diagnosis/wire-bending etc. Then we come to the logistics of implementation – most Ortho grad programs face challenges providing an adequate number of patients to train the residents. How are we going to find patients for the undergrads to treat? And, who will supervise them given the huge faculty shortage across the country, and then who will pay for additional faculty? The basics of orthodontic diagnosis and simple tooth movement are covered in most schools…treating full-fixed cases is simply not viable given the constraints mentioned before. It’s like asking undergrads to treat full mouth rehabs – not practical for the most part. A better option might be to offer special AEGD programs with an Ortho emphasis – the interested residents can then gain the knowledge they desire. Learning takes active effort and is unfortunately not an osmotic skill. There are far too may malcontents that complain, but were either simply disinterested when the information was presented to them, or disinclined to learn until other (financial) motivations came into being.
Hi Dr. Ulfr,
My letter to the AJO states a fact not an opinion based on the International Classification of Diseases and Related Health Problems-10. This compilation and classification has been a worldwide effort done by panels of experts (pathologists, epidemiologists etc.) For both ICD-9 and ICD- 10, malocclusion is classified a dentofacial anomaly. As an example a Class I malocclusion would have an ICD-10 classification M26.211.
You ask, “What, in your opinion, is the consequence of not treating this “disease””? My response is that the condition will not be eliminated or at least reduced.
I do have an opinion that not being designated a disease with an ICD code could prove problematic at least in the United States. Certain public and private programs involving public assistance, tax subsidy in the form of flex benefit plans, employer based insurance etc. could be at risk and challenged either in court or by the Internal Revenue Service of the US Treasury Department. Well anyway this is all moot because malocclusion is a dentofacial anomaly with a disease classification.
You discuss the difficulty in educating the predoctoral student. I certainly recognize this management/operations problem and suggest that schools can use expert consulting firms to evaluate and perhaps modify their curriculum. You also state “The basics of orthodontic diagnosis and simple tooth movement are covered in most schools.” I realize that posts in this blog are from all over the world and dental schools outside the United States may be teaching more orthodontics to their predoctoral students. The following is from a May 2015 editorial pertaining to American dental schools written by Dr. Rolf Behrents, editor-in-chief of the AJO and certainly a scholar of the highest repute:
“In terms of orthodontic education during dental school, few hours of instruction are provided for: the national average is approximately 95 total hours of scheduled instructions (i.e., less than 2% of the total hours of instruction). The time allowed for teaching orthodontics involves instruction in the classroom, working in a laboratory, and sometimes actually providing limited orthodontic treatment to one or two patients in the clinic. At some schools, as few as 11 hours of instruction in orthodontics are provided….”
This is kind of pitiful don’t you think? And forget about actually treating patients, the medical education model could be adapted where small groups of students could observe the orthodontic residents as they treat some cases. I would think that robust lecture hall didactic instruction to give the predoctoral student a real understanding of diagnosis, treatment planning, biomechanics, physiology etc. is not unrealistic. Then as these young dentists enter the practice world, even though they may never do any orthodontics (or endodontics or extractions etc.) but at least they could reinforce good orthodontic principles that are recommended by orthodontic specialists to mutual patients. As I tried to point out in another post, the family dentist could have a fairly close relationship with long time patients even on a personal level through friendship, children etc.
The best Orthodontics are done by GDP’s. It is the first practitioner seen by a young patient and where I live the specialists are generally not interested in treating children under 12. There are way too little specialists anyway and the economy does not allow many patients to afford them anymore. Sound interceptive Ortho are practised efficiently by GDP’s and their right to do ortho is not debatable. Parents google and find new trends in medical fields. It is not a given principle that they will choose a specialist anymore, they go where they get the best results for the best price. GDP’s should be trained to do extensive interceptive corrections of early malocclusions. If specialists are taking on the slandering of GDP’s in order to protect themselves from loosing patients, something must be wrong. I suggest that GDP’s get themselves on top of early intervention techniques with fixed appliances and make sure they know what they do. No one ever died from ortho treatment, not mentioning conservative ortho treatment and it is not restricted to specialists. Ortho IS dentistry and the most important part of it when it comes to children.
To make these sort of claims takes a certain degree of hubris, and as usual, all these claims of “best” are quite predictably unsupported. No one died from ortho treatment is invariably the excuse made by purveyors of treatment modalities of questionable efficacy and poor evidence. Simply not a standard to aspire for.
As a general rule… what is a good compromise?…
Never close the door on Ideal treatment should your compromise not work out. The best compromise is often NO treatment.
Unfortunately when money enters the mix, ethics sometimes disappears …
Yes they should. Provided that they have completed dedicated training in this subject. It is not easy to enroll on a specialist course therefore to become an orthodontist whereas there are some dedicated passionate general practitioners who became excellent in orthodontic treatment. Best regards. PK
Yes they should. Provided that they have completed dedicated training in this subject. It is not easy to enroll on a specialist course therefore to become an orthodontist whereas there are some dedicated passionate general practitioners who became excellent in orthodontic treatment. Best regards. PK
Greetings Dr. Winnick –
I understand the classification, but I don’t see the relevance as it pertains to orthodontic treatment. Where is the pathology, the cause-effect relationship, and what is the consequence of non-treatment? These are typical factors to consider with a traditional “disease”.
Your point re: additional didactic education is very well made, and one I totally agree with; however, dental school deans have been very resistant to allocate additional time to provide orthodontic instruction since this is frequently at the cost of restorative/perio/implants/endo etc. It would be fantastic to have dental students observe residents and faculty during diagnosis and treatment (I know several programs already do this), but again, we face time/schedule constraints.
Short of adding a year or so to dental school, a uniform level of knowledge (above and beyond what exists) is an uphill battle. You make some very good points, and I also believe that more (valid) education and engagement would enhance the quality of care. I would welcome a more open and encouraging foundation for dental students, but this needs to happen at the grass roots level. Thank you for sharing your thoughts.
Thank you, Kevin, for this opportunity to speak on this topic. I just retired from a full-time faculty position in the Department of Orthodontics at New York University. I started working at NYU in 2010 and retired in August 31, 2017. I was Director of the Predoctoral Invisalign Clinic starting in 2011. NYU College of Dentistry has 360-400 dental students per class. Even though this class size is very large, I think the students are trained well. I believe the college just received an outstanding accreditation evaluation this past October, after I retired.
The first year (2010-2011) I was there I provided some consults in the 14 general practice clinics and observed that dental students and general faculty knew nothing about orthodontics. I was the only orthodontist who had ever been on the general clinic floor. Even though the general practice faculty, perio faculty, and dental hygiene faculty were good in their own areas, they did not know how to evaluate the orthodontic needs of a patient. I was quite shocked. I had assumed that they could at least measure overjet and recognize a skeletal Class II patient with a retrognathic mandible. For years, the NYU Ortho department had been teaching in seminar and lecture many of these concepts, but dental students never had any hands-on experience where they really learned how to perform procedures on patients. Any patients who needed an orthodontic evaluation was referred to the Orthodontic Department.
Having had past experience in curriculum development and online training in orthodontics (www.ITICourses.com), when I was appointed Director of the Invisalign Clinic, I decided to develop an online basic orthodontics training program for the dental students. The online courses I developed were how to do an orthodontic exam, take records (exam, photos, alginate and PVS impressions, quick study models, some cephalometrics in the exam), do an analysis of records (problem list, diagnosis, treatment options), do detailed treatment planning for 5 desired outcomes by editing the ClinCheck tx plan with ClinCheck Pro 5, and then delivery of all treatment in the clinic. I did all of the ClinChecks with the dental students teaching them how to plan the treatment that would be delivered by the aligners. Then the students would perform all of these procedures in the Invisalign Clinic on their own patients from first identification to final placement of bonded chain retainers or removable retainers. Even though the students loved learning and performing these procedures, students felt they did not get enough credit for the amount of work they did. Often students would have to transfer their patient to another student or else they would be risking not having enough graduation credits, because the ortho credits were optional. CODA requirements focus on orthodontic space management, not examination and diagnosis of a patient who has orthodontic needs. This should be changed in predoctoral dental education since most patients have orthodontic needs.
This curriculum and Invisalign Clinic was a lot of work, but I wanted to prove to myself that online teaching could be 100% effective so that students could come into clinic knowing exactly what they were going to do. It took me 5 years to get it right involving the neuroscience of learning in my online courses and testing with tracking of student performance by SCORM Cloud. Unfortunately, I was not able to train other faculty using the online courses. I was able to train the residents over the last 3 years. So, after I retired the department decided to not use the online training any more. I believe one reason for this was because no faculty had taken the time to learn the online training and were not comfortable teaching it. Also, some ortho faculty and outside orthodontists did not want any “Invisalign” taught to dentists or dental students.
Politics plays a role in all education unfortunately. Practicing orthodontists (and many orthodontic faculty and department chairs) do not want to share their knowledge with general dentists. I took a lot of heat from orthodontists who heard I was teaching “orthodontics” to dental students. As I see it, I was helping dentists be better dentists and helping them help their patients have beautiful smiles. I don’t think a dentist can really achieve an excellent (healthy, esthetic, functional, stable, and enduring-wear free) result without orthodontics. However, if dentists and orthodontists are not properly trained to “look” to “see” these patient problems, they will not achieve an accurate diagnosis and treatment plan. All of us are unconsciously incompetent when we don’t know what we don’t know, until someone who has the expertise shows us how to do something in a better way. I believe most orthodontists specialize because it is fun to create a beautiful smile and help a patient be happier every day. If we share the basics of orthodontic knowledge, then dentists will be able to determine which patients can be treated by them and which patients need to be referred. Dentists don’t know how to do this now.
The good news is that it is possible to start changing dental education now. It will take 20 to 40 years to have an impact on dentistry world wide, but then more people will be happier, helping others, passing on the smiles.
why are orthodontists teaching only orthodontists, is orthodontics a closed society teach among themselves why don’t they teach orthodontics to GP dentists we don’t find this in other branches of dentistry , no body prevents a GP dentist from doing 3 RD MOLAR IMPACTION or RCT OR FPD ,implants if oral surgeon association comes with a statement GP dentist doing 3 rd molar impaction or implants is prohibited from doing so or endodontic society comes with advertisement that all RCT done by G P DENTISTS are wrong will it not look absurd , why is such a big secrecy in dissipating orthodontic knowledge some orthodontic societies even expel their members who teach orthodontics to GP dentists. it is irony that there are many many orthodontists whose main practice is implants , FPD , RCT . would all orthodontist restrict the practice to orthodontics just a wild thought