Adenotonsillectomy is better than RPE for treating paediatric OSA!
One of the most controversial areas of orthodontics is using orthodontic treatment to cure childhood breathing disorders. Strangely, some well-intentioned orthodontists promote this treatment in the absence of evidence. It has also been exploited by ne’er-do-wells and profiteers who take advantage of vulnerable people.
Over the years, I have advocated for better research on the treatment of childhood OSA. It should be more comprehensive than mere case reports or intentionally biased studies. So, I was pleased to see this new paper outlining a clinical trial.
A team from Brazil did the study. Paediatric Pulmonology published the paper.
Maria Cecilia Magalhães et al
Paediatric Pulmonology. Advance access https://doi.org/10.1002/ppul.27239
In the literature review, the authors noted that tonsillar hypertrophy is the most likely aetiological factor for paediatric sleep apnea (OSA). This means that the first line of management should be adenotonsillectomy (AT).
Some people suggest rapid maxillary expansion (RPE) as an alternative treatment to AT. Yet, RPE only changes the dimensions of the nasal cavity. It does not address the cause of obstructive sleep apnea (OSA). Despite this, some orthodontic advocates promote maxillary expansion as a treatment for OSA. Unfortunately, these claims are made without strong evidence to support them. The limited effectiveness of rapid palatal expansion (RPE) has also led to suggestions that it may be used in combination with adenotonsillectomy (AT) to treat OSA. Although, there has been limited research into this hypothesis.
What did they ask?
They asked this question.
“What is the best management sequence between adenotonsillectomy and rapid palatal expansion for non-obese paediatric patients with fully diagnosed OSA”?
What did they do?
They did a prospective cross-over randomised controlled trial with a 1:1 allocation ratio.
The trial was done in one dental school and the Otorhinolaryngology department. The PICO was
Participants
Children aged between 5 and 15 years with clinical symptoms of sleep-disordered breathing, tonsillar hypertrophy, and diagnosis of OSA considering outputs from nocturnal PSG that revealed an obstructive AHI of >1 event per hour. They also had maxillary constriction.
Intervention
Adenotonsillectomy
Comparator
RME with a Hyrax expander
Outcome
The primary outcomes were changes in AHI and MinSaO2.
The team calculated the sample size for a multiple regression analysis. They used a pre-prepared block randomisation and concealed the allocation using sealed envelopes.
They could not blind treatment to the operators, but they recorded and analysed all data blind.
One group of patients were allocated to get AT first ( AT1st). Then, after six months, the PSG was repeated. If this showed AHI>1 event, they underwent treatment with the alternative treatment (RPE). This is a standard cross-over trial methodology. The other group of participants had RPE first (RPE1st). Then after six months, they were offered AT.
This is a standard cross-over methodology.
What did they find?
Thirty-two participants entered the trial. They randomised fifteen to the AT first group, and 17 to the RPE first group. At the end of the first six-month period, they treated 15 of the AT1st group with RPE. While, 15 of the RPE1st group received AT.
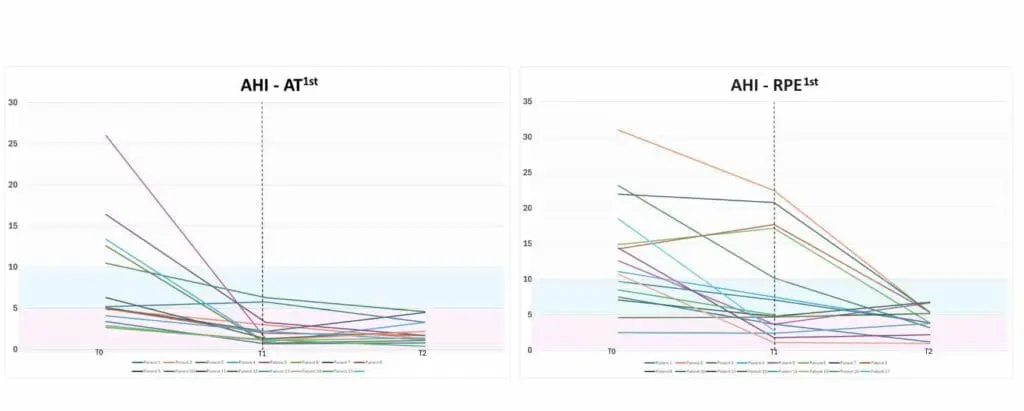
The team presented data for inter and intra-group values of the two primary outcomes. This resulted in a large amount of interesting data. I thought that these were the main findings.
- The combined consecutive use of AT followed by RPE resulted in a mean improvement of AHI from 8.08 to 2.13 and 12.6 to 4.05 in group RPE1st. Most of the AHI reduction was due to the AT. This suggests that RPE has an irrelevant effect when done after AT. RPE alone results in a reduction of less than half of the initial AHI.
- The regression analysis suggested that the AHI reduction was explained by the initial AHI and the use of AT first. The effectiveness of the AT was directly related to the severity of the AHI. In cases where the AHI was severe, the AT reduced the AHI. However, its effect was more limited when AHI was mild or moderate.
- When they examined this for RPE, they found that it had a lower capacity to promote a reduction in AHI.
- Similarly, for MinSaO2, the most significant improvements were found when using AT.
The authors produced this great graphic which clearly shows the relative effects of the interventions on AHI. I would like to thank them for letting me include it in my post.
Their conclusions
The study team suggested that AT be used as a first-line treatment for children with severe AHI. RME could be used as the initial treatment for milder cases, followed by a watchful wait before considering AT.
Notably, none of the patients had an AHI of <1 after the first treatment. In effect, they were not “cured”. This is also an important finding. The authors pointed out that patients should be informed that the treatment can reduce the severity of AHI. However, it will not necessarily cure OSA.
Their conclusions were
“Most AHI reductions and MinSao2 improvements were due to AT. Therefore, RPE as the first line of treatment is not warranted”.
What did I think?
This was a well-executed small RCT. The team closely followed standard trial methodology. Importantly, they used relevant outcomes and conducted a multivariate analysis to account for confounders. It provides a high level of evidence.
The team mentioned some limitations of their study. Firstly, they did not include an untreated control group. This would have helped them understand the effect of natural growth on their outcomes. Additionally, they did not assess the participant’s quality of life. It would be valuable to include this information in future studies.
This study offers clinically relevant information. Importantly, it emphasises the consensus that adenotonsillectomy is the primary treatment for OSA, and RPE may not be beneficial.
This study further supports the argument against orthodontic treatment for breathing issues made by some orthodontists and dentists. This conclusion is likely to spark intense debate. Let’s keep the discussion civil and also remember the pyramid of denial.

Emeritus Professor of Orthodontics, University of Manchester, UK.
These conclusions could be made a decade ago with the research available then
Thank you Dr. O’Brien, for considering this valuable article.
It is a very important study, but the authors misjudged the results and therefore reached the wrong conclusion.
“adenotonsillectomy is the primary treatment for OSA, and RPE is unnecessary”
The first part of this conclusion is valid, but the second part (RME is unnecessary) is a misinterpretation that goes beyond its purpose.
Some of these pediatric OSA patients have a narrow upper jaw due to hypertrophic adenoids. Adenotonsillectomy is the treatment of one of the etiological variables, while RME is the treatment of the result.
The first step of treatment in pediatric OSA patients is adenoid, tonsil, etc. is the surgical removal of the areas. If there is a posterior crossbite, RME must be performed in this case.
Thanks for the comments. I have changed my interpretation in the blog post, as I think that I was too blunt. It is interesting that you feel that the patients had a narrow upper jaw because of the hypertrophic adenoids. I am not an expert on this, but I have not come across any papers that support this hypothesis. Can you let me have a reference and I will include this in future discussions.
Dr O’Brien thank you for your kind response and the correction.
The effect of the Functional Matrix Theorem on the development of craniofacial structures is a fundamental topic we teach our students. According to this theorem, the position of the tongue directly affects the formation of the upper jaw. When the position of the tongue is displaced downward as a result of adenoid hypertrophy in children, the maxillary arch form is affected by this situation.
In addition, in the “Soft Tissue Tension Hypothesis” presented by Solow and Kreiborg in 1977, craniocervical posture, which is directly related to the tongue position, is a factor that plays a role in the development and function of dentofacial structures.
In addition, there are studies by Linder-Aronson, in particular, that examine the relationship of the adenoids with the maxilla and other orofacial structures.
When the literature is examined, many more studies can be found on this subject.
These are the first ones that come to mind.
Solow B , Kreiborg S. Soft-tissue stretching: a possible control factor in craniofacial morphogenesis. Scand J Dent Res. 1977 Sep;85(6):505-7.
Linder-Aronson S. Adenoids. Their effect on mode of breathing and nasal airflow and their relationship to characteristics of the facial skeleton and the denition. A biometric, rhino-manometric and cephalometro-radiographic study on children with and without adenoids. Acta Otolaryngol Suppl. 1970;265:1-132.
Linder-Aronson S. The impact of adenotonsillectomy on the dentofacial development of obstructed children. Eur J Orthod. 2018 Jul 27;40(4):451. doi: 10.1093/ejo/cjx097.
Linder-Aronson S. Effects of adenoidectomy on dentition and nasopharynx. Trans Eur Orthod Soc. 1972:177-86.
Sökücü O, Okşayan R, Uyar M, Ademci KE, Üşümez S. Relationship between head posture and the severity of obstructive sleep apnea. Am J Orthod Dentofacial Orthop. 2016 Dec;150(6):945-949. doi: 10.1016/j.ajodo.2016.05.011.
O’Ryan FS, Gallagher DM, LaBanc JP, Epker BN. The relation between nasorespiratory function and dentofacial morphology: a review. Am J Orthod. 1982 Nov;82(5):403-10. doi: 10.1016/0002-9416(82)90189-0.
Dear Babacan,
Thank you for your valuable information about this topic.
Many orthodontist are not aware of this point… ın the year 1970’s you have shown these articles..
We may need to focus and begin again by working Medicine department to follow the affects of Rme..
Many pediatricans sent me children to observe childrens maxilla..
They say please open the maxilla othervise they have to use many antibiotics..
I hope we have to begin work with these pediatricans together to see the affect of Rme objectively..
Dr. Sökücü, I completely agree with your comments and suggestions.
In addition, ENT doctors should be open to cooperation on this issue. Patients who need adenectomy and tonsillectomy should be referred to an orthodontist for consultation after the procedure. I refer all children with maxillary narrowness, difficulty breathing and snoring to an ENT doctor for consultation.
Dr. O’Brien,
Thank you for sharing this article. I tend to fall into the more conservative group when it comes to OSA, and maxillary expansion so please understand my bias. Having said that, however, the PICO selected participants with AHI > 1/hour AND MAXILLARY CONSTRICTION. If there was maxillary constriction (and orthodontics has pushed correcting problems in all three planes of space), why would we not try maxillary expansion first? If it were my child (or now grandchild), I would certainly want to try less invasive procedures first. I understand maxillary constriction does not equal posterior crossbite but if it happens to reduce AHI (as some did in your graph), this would be a big win for the family. In addition, did you look at how many patients increased their AHI after the second intervention? It appears that many (maybe even the majority) did so in both experimental groups. What does this tell us?
John
Thanks for the comments and you make good points. While it is worth going for the most conservative option. It is clear from this study that the more severe the OSA the greater chance of correcting this with AT. If they were my child or grandchild, I would hope that they are given information from this study and others so that they can take an informed decision. This is the main value of this study.
“I understand maxillary constriction does not equal posterior crossbite but if it happens to reduce AHI
(AS SOME DID IN YOUR GRAPH)”
A control, untreated sample, would have been wonderful to superimpose or interpolate the benefit of either intervention but in particular RPE, when the AHI may be, to a degree, cyclical (environmental exacerbating factors, etc.) and the improvement explained perhaps by cyclical oscillation.
Dear Sir,
Thank you very much for the informative post.
Hopefully the future studies can shed some light on natural improvement in breathing as the child grows (as pointed out by you in the summary) and also factor in habitual mouth breathing in some cases owing to prolonged phases of nasal obstruction due to one reason or the other.
Thank you.
Yours sincerely,
Mr Karun Sagar
Your timing is impeccable, Kevin. In September, the FDA gave a palatal expander approval for the treatment of pediatric OSA. It is the first palatal expander to join the plethora of MADs for adult OSA. The point is, all palatal expanders are not alike; they show significant heterogeneity in terms of design, materials and protocols. I teach my Fellows and Residents that, in these cases, the guiding principles are: site, severity and collapse. In this study, the site of airway obstruction was the adenoids and palatine tonsils. So it makes sense that adenotonsillectomy was the treatment of choice. On the other hand, if the tonsillar tissues were less hypertrophied but there was significant maxillary constriction, it could be argued that “palatal expansion” might have been the preferred option. In either case, the enigma lies in the clinical response/behavior i.e. how was upper airway collapse prevented, using the AHI as a surrogate.
Disclosure: I am the inventor of the palatal expander referenced above
Without question, a non-surgical approach would be preferable. If that approach has positive results for airway / sleep apnea, certainly everyone will be delighted. The issue could easily be lack of clear communication with the parents. If the parents understanding is that an expansion, nonsurgical approach “may be effective”, have paid time and money for that result and the procedure does not produce the desired response, what is the parents understanding of the next step and the cost as well as risk/benefit ration for the added procedure(s)? Have the parents been encouraged to seek additional opinions and made an informed decision? Has adequate written informed consent been obtained? Do they have unrealistic expectations?
There are many upsides to this research. The first is that it was a prospective randomized trial. This has the advantage over retrospective trials, with their inherent bias. Also important, as there have been cases of this used as contrary evidence, patients with cleft palate and craniofacial syndromes were not included in their data sets.
The second is that polysomnography (PSG) was used to determine the apnea hypoxia index (AHI) and thereby the presence or absence of obstructive sleep apnea (OSA). Far too often alternative inaccurate methods are used. Questionnaires, clinical examination, and radiographs such as CBCT are fine and appropriate for screening purposes. However, they are appropriate for screening purposes only. They cannot determine the truly important information, the AHI, and they are not diagnostic for OSA. With research not utilizing PSG pre and post treatment, it is far too easy to diagnose a condition which does not exist. Then a change which may or may not have been of any therapeutic benefit to the patient can be claimed to have improved a problem which may not have existed.
PSG remains the gold standard in diagnosing AHI and OSA. I personally am highly suspect of any research which does not use it pre-treatment, post-treatment, and also at an additional sufficiently later post treatment time point.
The third is of course that it addressed the ad hoc argument that expansion is valuable as an adjunct to the removal of tonsils and adenoids (TA). Ad hoc hypothesis is used when the primary hypothesis is proven wrong. The ad hoc part is that claim “it would have worked had they only done this”. While ad hoc hypothesis can be appropriately applied, to be logically valid it must presumed wrong until proven otherwise. The burden of proof is with the one making the ad hoc claim.
In this case the primary argument is that palatal expansion treats or prevents OSA in children. IMO, this has now been sufficiently disproven in the valid literature. In response to this, there has arisen the ad hoc argument that “expansion is a legitimate adjunct to TA or a legitimate substitute if TA fails”. This research would appear to be a nail in the coffin of the ad hoc hypothesis that expansion is helpful after TA has been done.
To look at the weaknesses in this research, while it is an admitted weakness, the absence of a control group is still a weakness. This is especially the case as children are being studied. Children are constantly growing and changing. A change attributed to some treatment we provide might have occurred anyway without any interference at all on our part. We have already seen the research showing that “watchful waiting” or doing nothing, is equally effective as palatal expansion in the treatment of OSA for children.
So, a control group, while valuable for all research, seems especially appropriate for children. My best guess is that as these were patients who were diagnosed with issues with their AHI, doing nothing was not permissible within the ethical boundaries of the research.
There seems to be so much research disproving any benefit to children from expansion as a means to treat or prevent OSA, it must be considered why this information is still being spread. There are still some lecturing, providing courses, and offering “coaching” who advocate for expansion as a treatment for OSA, and sometimes even a primary treatment. Within that group, there does seem a consistent financial incentive to continue to push this treatment despite what is becoming overwhelming valid evidence against it. Their only tool is expansion, the proverbial hammer. Every possible cause of OSA seems to then be considered their nail. We gave heard this theme music played before in orthodontics.
Those following these Pied Pipers might take warning from what happened to those who made and sold the AGGA appliance. What will be the reaction when the FDA comes in to regulate and fine, as they have with those who made and sold the AGGA appliance as useful? Will there be class action lawsuits against the doctors who do this treatment for that purpose, as there has been with doctors who used the AGGA appliance? Perhaps even more important to a practice financially is to consider, what would happen when a major news organization decides to do an expose on the recommendation of palatal expansion to treat pediatric OSA? Would we want to be the doctor who recommended this when parents themselves have heard that this recommendation was not justified?
Dr Kazmierski:
In response to your question “what would happen when a major news organization decides to do an expose on the recommendation of palatal expansion to treat pediatric OSA?”, please note my reply above and https://aasm.org/fda-clears-vivos-oral-appliance-for-children/
In the 1980’s George Meredith, MD, was a big proponent of combining AT surgery and RME use. In fact he often preferred RME treatment prior to surgery as it made his job easier. As editor of the Journal of Ear, Nose and Throat he was instrumental in devoting 2 entire issues of that monthly journal to the airway/ dentofacial relationships back in the summer of 1986.
He was a big proponent of measuring back in the days before computers and he had reams of data showing the benefits of combined therapy. It would be interesting reading to contemporary researchers. When I practiced I followed his combined therapies route for most cases. AS CBCT became available I found the data supportive of my practice.
Studying laminar flow/analysis we can extrapolate the anatomical strictures as a resultant remnant of poor growth. From current data one can infer the interrelationships from the “old” data and ‘new” data and see that the single modality treatment has limitations. I believe that this analysis needs to be studied more as it might make a change in the approach to improve airways surgically. I found that the obvious was not always the approach that resulted in the best desired result. As noted above, none of the results “cured” the patients. Also the results are skewed by the patient base. So to say that neither are effective is improper interpretation of the data. I, and I sum others , have used these techniques and seen life changing results in our patients and not so much in others. Obviously, further knowledge needs to be accumulated.
The study appears to have some merit, but I think the most important thing is that both approaches are nothing more than “tools”, and that we have to be knowledgeable of when to use them, timing , and followup, and proper education and consent.
This study cab NOT be taken as a definitive study, but one of useful information.
Thankyou for reviewing this interesting article which provides some ,very useful,additional information on the “Airway issue”
I find this area difficult to understand and apply to everyday practice and all comments/help are much appreciated by me !
I note that this study descibes its subjects as non -obese with balanced maxillomamandibular relation.
My experience in Canada is that most referral pts.already have a skeletal dysplasia when referred.In addition,unfortunately,childhood obesity is becoming ,evermore,common.
Perhaps ,most importantly importantly there is a great reluctance for ENT,s to co- operate with removal of tonsils/adenoids even in very severe OSA situations.Surprisingly to me ,most ENT,s are reluctant to even read the “dental”literature on this topic ,even when presented to them by orthodontists!
I believe the above prompts many of us to use RME as it is “the only tool to address OSA ,in particular,available to us!
Thanks,again.
Just a few of my thoughts. I attempted to access the article but was unable to do so—did they evaluate the amount of expansion as a variable? Additionally, has anyone conducted a similar study using MARPE appliances? Were factors such as age, sex, or CVM stage considered in their analysis?
It seems like these would be critical considerations to address before drawing conclusions about effectiveness or making broader recommendations to healthcare professionals. While I’m not an academician—particularly when it comes to understanding the statistical analysis section—my primary goal is to do what’s best for my patients. I am open-minded and curious, always striving to learn and improve my understanding. I am concerned about the potential for misrepresentation of the role of RPE in these cases. That said, I recognize that I could be mistaken, and RPE may indeed not be as beneficial as some of us have hoped.
Thank you in advance for your consideration and response.
Sincerely,
Jay Burton