Back to Basics: What do we know about clear aligner treatment?
In this series of extra posts, we return to the “Back to Basics” posts by Martyn Cobourne. This time, he will cover the evidence on clear aligner treatment. This first post is concerned with the effectiveness of tooth movement with aligners.
Tooth movement and aligners
The data relating to the clinical effectiveness of aligner tooth movement is mainly based upon small volume retrospective or prospective clinical studies, which generally compare digital treatment predictions with digitally achieved outcomes using regional superimposition techniques on the dentitions.
Aligners rarely achieve the predicted tooth movement, and the effectiveness of aligner treatment will vary depending upon the type of tooth movement being attempted and the type of tooth it is being attempted on.
We have summarised the data below based on relevant systematic reviews (Rossini et al., 2015; Robertson et al., 2019; Koletsi et al., 2021) and where not explicitly covered within these systematic reviews, the most contemporary original data (Simon et al., 2014; Haouili et al., 2020.
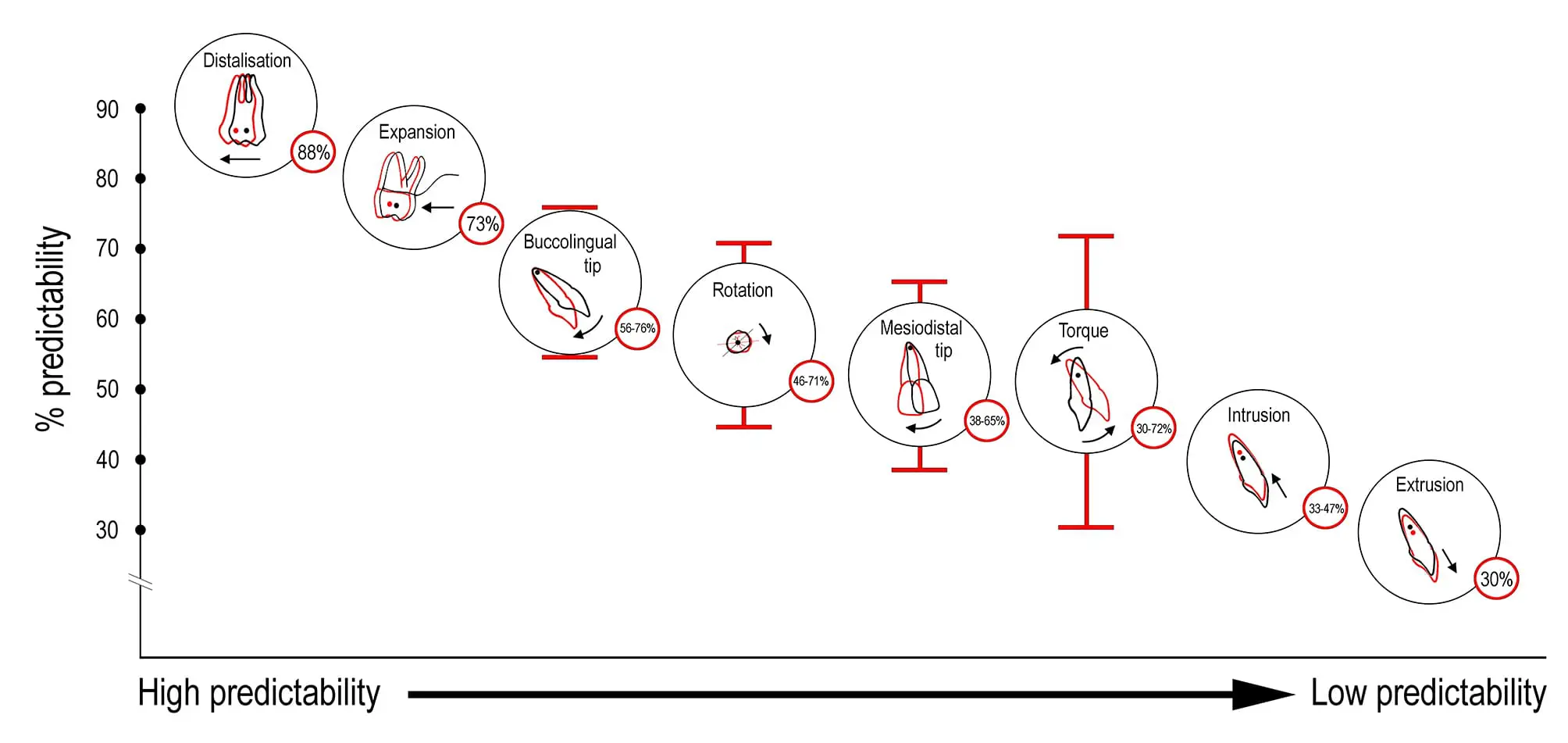
We have also presented the data in this graphic.
The data
These data relate primarily to the Invisalign® system, and as you can see, there is wide variation in reported effectiveness. It would also be nice to categorise data on effectiveness relating to each type of tooth movement and tooth, but the data is not there.
- Overall accuracy for all tooth movement using clear aligners is around 50% (Haouili et al., 2020) and significant differences between predicted and actual tooth movement should be expected; however, these differences in predictability depend upon the type of tooth movement,
- The predictability of tooth movement seems to be improved if the aligners are changed every 2 weeks (Castroflorio et al., 2023);
- Maxillary molar distalisation has a reported predictability of 88% (Simon et al., 2014), with the movement of 2-3 mm seemingly achievable, although the evidence base is very low (Verma & George, 2021);
- Expansion of the maxillary and mandibular dentition is associated with 73% and 88% predictability, respectively. The tip is more predictable than bodily movement, and predictability generally gets worse from canine to first molar; expansion of around 1.5 mm is achievable (Houle et al., 2017; Zhou & Guo, 2020);
- Buccolingual tipping accuracy is around 56% overall, extending up to 76% for labial tipping of the maxillary lateral incisor (Haouili et al., 2020);
- Rotational accuracy ranges from 46-71%; canines have the lowest percentage accuracy (48% for maxillary; 50% for mandibular) and mandibular incisors and premolars the highest (71% and 67%, respectively) (Rossini et al., 2015; Haouili et al., 2020; Koletsi et al., 2021);
- Mesiodistal tipping accuracy ranges from 38-65%, with mesial tipping of the mandibular lateral incisors being the least accurate and mesial tipping of the maxillary second premolar the most accurate (Haouili et al., 2020);
- Torque for the maxillary central incisor ranges from 30-72% with an average of 51% (Simon et al., 2014);
- Intrusion is achieved with an accuracy ranging from 33-47% (maximum accuracy for maxillary and mandibular central incisors; minimum accuracy for maxillary lateral incisors); an average amount of 0.72 mm true intrusion was generally attempted (Haouili et al., 2020; Rossini et al., 2015);
- Extrusion is one of the most challenging movements for aligner systems to achieve (only 30% accuracy overall), with the lowest accuracy associated with maxillary and mandibular central incisor regions (18-25%, respectively); an average amount of 0.56 mm extrusion was generally attempted (Rossini et al., 2015)
- Regarding the irregularity index, a decrease of 4-5 mm in the incisor regions is achievable with aligners (Rossini et al., 2015).
The next of these posts is on the effects of attachments on aligner efficiency.
Martyn Cobourne is Professor of Orthodontics at King’s College London. He also runs the excellent Evidence Based Orthodontics Facebook Group and the Evidence Based Orthodontics Course.
Bibliography

Thank you Martyn for the nice summary. In my experience, where it get tricky to combine results for different studies is the knowledge or lack off if the clinicians treatment planning did or not exaggerate the expected movements aware of the potential limitation of the planned movement. In other words, they may have overcorrected by 50% a specific tooth movement in which case a final result showing a 45% correction could be considered successful.
Carlos – I agree. But I also find that caveat very misleading. Of course it is a favorite of all the Invisalign KOL’s. They often state that they plan “force systems” and not “final tooth positions”.
However, as any clinician knows, the issue with some moments like extrusion and PM rotations is the loss of attachment engagement. Once it is lost, there’s no hope. So if a maxillary lateral incisor needs to extrude 2mm – there’s no point in extruding it 4mm on the clincheck with the hope of achieving 50% movement. The tooth will extrude only until the attachment stops tracking. So doing a “force system” actually makes no sense in that instance. If the attachment stays engaged, you’d actually been in a bad situation.
The same goes for a PM rotation – there’s no sense in over-rotating, since it will only rotate until attachment stops engaging. You might want to over-rotate a little just because of “relapse potential” but if a PM is rotated 30 degrees you aren’t going to plan 60 degrees in the hope to achieve half.
Of course, for some movements – like expansion – it does make sense to over compensate. But for me those darn anterior extrusions (esp. max laterals) and PM/Cuspid rotations are the most frustrating aspect about aligners.
You’ve articulated what I’ve been wondering about those clinchecks that are grossly overcorrected. Also some teeth respond 90% and some 50% but you can’t necessarily control which ones, so designing overcorrection can be difficult.
Yes, this makes sense, Shawn. The biomechanical response is multifactorial. My point was about how the reported percentage of change should be considered based on what was initially planned. Not if the initial plan was reasonable or not. Martyn is to discuss attachment design in the next blog. Clinical experience should help us decide what type and amount of specific tooth movement is highly unlikely to work out. Clinical uncertainty always exists to different degrees. A hybrid approach is a more reasonable approach for a lot of the malocclusions.
I respectfully disagree with the math logic in your comment, according to your logic, 50% of the designed movement is considered desired movements, and 50% is overcorrection. This means 100% overcorrection as a method of aligner setup. I can’t imagine any practicing doctor adopting such extensive overcorrection.
Fair point. I intended to raise the point that what is reported as a percentage of change may represent change related to the planned movements, which may have a degree of planned overcorrection based on the uncertainty of the system. I could have used a smaller percentage of planned overcorrection to make the same point.
I wonder why some orthodontists try to treat all their cases with clear aligners despite all these restrictions on tooth movement. As the name suggests (Clear Aliner), these devices are originally aliner. The best they can do is to treat simple cases of crowding where there is no problem in the sagittal and transversal directions. It is not ethical to try to present this method as the new gold standard in the treatment of complex cases that use more aliner, extra attachments and take longer duration to treat, even these cases can be easily treated with fixed orthodontic appliances. Moreover, since these appliances have limitations even in simple tooth movements, it is not right to try to treat every case with this method.
*VV provides lectures for Align Technology, Manufacturer of Invisalign System.
Thank-you Kevin and Dr Cobourne. A few comments if I may?
Firstly, as researchers, I believe it is imperative to be specific and accurate with terminology if we want to claim any validity in reported data. So, when we present a title “What do we know about clear aligner treatment?”, or “tooth movement with aligners”, I feel that this this is non-specific to the point of being misleading. We have literally hundreds, perhaps thousands of aligner systems and they are not the same. Only 1 computer aligner system is currently evidence based, to the extent that you may present this blog based on “systematic reviews and contemporary original data”. The programming – some still manual, some digital (computer), velocities, materials, trim, mechanics (attachments, staging) and prescribed use are just some examples of the variables that make lumping these appliances into the same research question fallacious. You do make the point midway in your report that these data relate mostly to the Invisalign system. If not, they should be excluded when asking the type of questions that you are looking at – mainly degree of expression of programmed movement. As you say, there is very little, if any publication on other (major) aligner brands. Invisalign remains the only “evidence based” aligner system in 2023 and it took 25 years to get to this point, despite the specialty and profession at large screaming for “evidence” from day 1 – and rightly so. It seems other aligner companies can slip into your research summary above and not be held to any level of accountability by its users or require an evidence base – even case reports would be a start. I hope that information is passed onto patients. Are other systems just cheaper, different materials, longer, shorter, clearer, fewer attachments more attachments, worn for 14 days, just overnight ….and these “innovations” and price difference suddenly makes them the same or better? Thanks to our sloppy and biased tendency to group together all “aligner tooth movement” (would we ever do that researching bracket and wire systems? ) and the blind trust that we have in bracket manufacturers who have curiously turned to aligner manufacture, somehow it is suddenly OK for clinicians to treat with a non-evidence based appliance because it “looks like” the other one that actually now has a body of evidence!
I do love the graph and have attempted similar in table format. What I am waiting for – and you know I have asked for in this blog for many years – is the same data set using fixed appliances. Now that digitally programmed fixed appliances are readily available and have been for many years, I am curious to see the same outcome protocol applied to those mechanics. My gut tells me they will have similar shortfall of programmed movement especially for torque, intrusion, levelling curve of Spee, rotation without re-bonding (or analogous second series of aligners). Because response is due to anatomy and physiology as large variables and not only on the material ability to deliver a force system. We could not claim to be scientists or to allow for laws of physics and engineering to expect 100% of programmed movement to be expressed by any mechanical device that abrogates data in many steps; from digital to analogue and then into a most variable biological specimen, and we have all re-bracketed and overexpanded / over torqued archwires due to this same mechanical “shortfall”. Why do we rarely if ever use these terms when discussing fixed mechanics “shortfall”, “accuracy”, “predictability”? Ahhhh – because we could never measure these things until Align Technology pioneered tooth moving software, allowing digital fixed appliance systems to also evolve. The graph may look different – for example the extrusion would likely swap places with distalization. Expansion is likely similar…but we don’t know! I would have thought that we should have been screaming for this available data if we claim to be an evidenced based specialty and that fixed appliances are / were / we don’t know – still gold standard? Measuring outcome of pre-formed wires with no re-bonding against a pre-determined outcome is analogous to the clinical studies you quote above; most not measuring the ability of computer programmed aligners – or let’s be accurate– the Invisalign computer programmed aligner system – to help obtain a high quality outcome (as to finish in 1 series of aligners especially in moderate to severe malocclusion is unrealistic due to physics and engineering) ; all they measure is the degree of expression of programmed movement – data we don’t have for fixed appliances but readily could have, thanks to Align Technology’s innovation , development and expiring patents in digital tooth moving software.
Regarding frequency of aligner change, I am not sure that based on 1 (albeit good) paper looking at so many variables (similar to Clements so long ago but with different material) – if with the ultimate sample size of 26.3 subjects assuming equal distribution in the 7, 10 and 14 day protocol that we may conclude that for certain movements we “need” 14 days aligner change. This conclusion becomes particularly risky taking into account other research has shown no significant difference between protocols, that very little activation remains after 7 days and lag phase is not significant in contemporary biology of tooth moving studies, that activation and manufacturer recommended use of the system we are supposed to be testing in terms of efficacy (as opposed to clinician modified) remains 7 day aligner wear and that practically, in the field, most clinicians treating moderate to severe malocclusion with the Invisalign System will use at least 1 AA series to come closer to the pre-determined outcome (and thus decrease or negate the average 12% discrepancy in certain movements found by the authors). It will also be welcome when we use non-programmed segment of teeth and / or rugae to superimpose rather than “best fit” with Geomagic, as per Newby (2010) if we really want to talk expression of movement in individual tooth groups.
Looking forward to the next post -evaluating the “effects of attachments on aligner efficiency”, or possibly “the efficacy of Invisalign attachments” as summarized from the available literature. I do hope that we may report data from samples where no doctor input altered duration of aligner wear, decreased velocity or modified staging as these are the variables that determine the engineering of these forms. I am not aware of such a “pure” sample. Perhaps we can really get back to basics and measure the degree of expression of various digital arch wire systems?
Finally, a question Kevin, re your post of November 20. At what point does a clinical researcher presenting their findings evolve into a KOL?
Ms or Mr VV, it would be nice to identify your name and area of research interest, since you declare yourself as a researcher at the beginning of your comments …. that would be more ethical instead of identifying yourself as a KOL for Align!
Apologies! I identified myself as a KOL for Align as I believed that was the relevant information for the reader to easily identify a potential source of bias. (although I am still confused about the definition of a KOL and the transition of a clinical researcher to KOL. )
My name is Vicki Vlaskalic. I am an orthodontist now practicing and teaching in Melbourne Australia. In 1997, together with my visionary Chair ,Professor Robert (I was Assistant Professor of Predoctoral Orthodontics at Pacific in San Francisco at that time) I co-designed the initial feasibility study and co-authored the initial publication on an appliance that eventually became “Invisalign”. My research interests include quality of orthodontic outcomes (my thesis was in the Australian weightings of PAR index) and have published together with Professor Sheldon Baumrind, Dr Don Poulton and Professor Stephen Richmond on outcomes in various modes of orthodontic practice, I prepared research grants at UCLA with Dr Patrick Turley on protraction face mask with and without RPE and once arriving at UOP (Pacific) root resorption was also in my research and peer -reviewed publication repertoire. I was fortunate to receive 3 AAO research and teaching awards and currently teach at the University of Melbourne where I have mentored 4 related Masters thesis (starting in 2010) using Geomagic and CBCT analysis to measure expansion degree and type of movement with Invisalign in both adults and teens. Since 1997, I present my own clinical and research findings regarding Invisalign at universities, independent academic meetings as well as company sponsored events. I have purposely never been an employee, never owned shares, nor family members, in Align Technology (unfortunately!). But yes, I am biased, as we all are. I am proud of my 26 year role in assisting development of the innovations that have allowed our increased cohort of patients, specialty and profession at large to benefit- whether they choose to use the Invisalign system or not – and to make its largest leap in innovation over 120 years and to benefit from the advent and determination of Align Technology in pioneering and introducing digital technology including iTero and digital workflow models to our previously purely analogue world. I am sure you may find my CV if you require elaboration. Thank-you
Thanks for this comment. I have been having a look at the literature on KOLs and it is confusing. I cannot help thinking that this is a screen of smoke and mirrors. I looked back at some academic defintions and here is a clear one “KOLs are physicians or non-physician scientists who are engaged by pharmaceutical companies to act as consultants to the companies but also to influence doctors’ medical practice, including (but not limited to) their prescribing behaviour”. They are also frequently paid to carry out this role. However, the important concept in this is declaration of a conflict. This is easy. If someone is being paid by a commercial organisation they are a conflicted KOL. I hope that this answers this point.
My name is Naphtali Brezniak. On July 1986 I graduated UOP ortho program. Later I became the head of the ortho department in one of the hospitals in Israel. The late Dr. Poulton was then the head of the department, and Prof. Roberts was and still is my mentor. At the beginning of the century, I became an Invisalign (CA) fan, however, due to a deep study of biomechanics I found that at least for me, it does not serve my professional goals. The need to use fixed appliances at the end of most treatments, pushed me to investigate the new promising appliance. The 1st article I published was about the CA inability to develop a couple. The truth is that at that time I did not truly understand this magic movement and its full incorporation into the treatment. Since then I studied it as I realized that, unlike Burstone and Smith’s iconic article where they defined different tooth movements, there is another way to do it according to the number of points applied to the teeth. One point force application develops tipping with the center of rotation of the movement at the center of resistance of the tooth, unless the vector is passing through the center of resistance of the tooth, where it develops bodily movement ( with the center of rotation at infinity). Two points force application, the couple which is unique and actually the magic movement aligners cannot develop as ortho movement, and its center of rotation is in the center of the couple. This special article was published lately in the Angle Orthodontist, Vol 93, No 5, 2023 – Clear aligner biomechanical limitations: anchorage and couple (torque) development. by Naphtali Brezniak; Atalia Wasserstein; Noam Protter. Three-point force application is the combination of one and two-force applications together, which develops the walking movement we miss in aligners but it develops automatically (nobody needs to do anything about it) in Fixed appl. treatments.
Therefore I was surprised the see the above drawing as well as the high predictabilities of movement CA cannot accomplish, for example, bodily movement. My second point is: what is the meaning of overcorrection. As far as remember in orthodontics we need to correct and not to overcorrect. (Don’t forget to overcorrect and much more: The current finite element analysis publications related to clear-aligner treatments (Naphtali Brezniak and Noam Protter, AJODO Oct 2023).
I believe that we need more RCT studies done under the supervision of ortho departments. I believe that there are much more to study. True, we are in the 8th generation of the aligners and the predictability was supposed to be by that time almost 100%, but it is not? Why? I believe we have to begin with studying the anchorage first and then continue to the study the appliances. We have to remenber Angle and Brodie who both denied the use of removable appliances back in the 1920, for those reasons.
I’m not a KOL of any professional orthodontic company.
As a “x-KOL” who was compensated for sharing research and clinical experience with practicing colleagues, I ADMIT it was a mistake. My experience proved to me that for-profit corporations are never motivated to finding the truth through research, they are only interested in hand picking evidence that can produce more sales and financial returns.
It is very difficult for any well meaning researcher to see the above fact, I empathize!
Kevin,
This concern with KOLs has gotten overheated. I believe you have conflated the KOL, by American healthcare standards, with the Key Influencer. The KOL primarily presents education, e.g., research and clinical findings, and is held in high regard. The KOL may become an influencer, but this is secondary to their primary purpose. The Influencer is primarily associated with marketing, which unfortunately may be misleading. This is where your criticism should be directed.
Thanks for the comment. Sorry for the confusion. I have defined the KOL using an international definition. This is a person who receives funds from a commerical organisation to advise on treatment and give lectures on the treatment. The main factor that differentiates them from researchers is that they receive funds from the commercial company. As soon as they get paid they are conflicted. I hope that this clarifies the situation.
I have been having a look at the literature on KOLs and it is confusing. I cannot help thinking that this is a screen of smoke and mirrors. I looked back at some academic defintions and here is a clear one “KOLs are physicians or non-physician scientists who are engaged by pharmaceutical companies to act as consultants to the companies but also to influence doctors’ medical practice, including (but not limited to) their prescribing behaviour”. They are also frequently paid to carry out this role. However, the important concept in this is declaration of a conflict. This is easy. If someone is being paid by a commercial organisation they are a conflicted KOL. I hope that this answers this point.
Thanks Kevin – any clinical researcher / academic who presents at any commercial meeting, or “academic” meeting sponsored by the product they are investigating , and / or receiving honorarium, directly from the company or via the professional body holding the sponsored meeting is a KOL by that definition. Or it is OK to ignore the “middle man” for payment? Very broad – “frequently paid” – does that mean any honorarium ? Even academic / professional body meetings would fall into that category for every speaker presenting research on a “product or service?” The addition of the caveat “paid to influence doctors” speaks to Dr Winnick’s relevant and enlightening comment above. The KOL as you describe above has been part of our specialty since its dawn, Personally, my education and clinical experience benefited from KOL’s, Angle, Andrews, Roth, Ricketts, could go on. When you hear the BS, you call it out, (was not fun with Ricketts, Andrews more humble). As discussed in previous blogs, we should be educated enough to be curious, to question respectfully and to discriminate between baseless marketing and hierarchy of clinical evidence.
Few years ago, I decided to transform my clinical workflow from a mix of 50/50 fixed appliances and aligners to become 100% aligners, and to facilitate this transformation I used a commercially available generic brand and its platform, let’s call it Company-X, I took on all treatment design tasks, but delegated fabrication tasks to Company-X, setup technicians were NOT allowed to touch any of my cases.
Since Company X (and pretty much every other aligner company in our space) is being managed by a handful of smart engineers, I understand and empathize how difficult it might be for these non-doctors to understand the clinical and scientific concerns doctors have regarding aligner solutions. I will try to present my concerns in “engineering lingo” hoping this may deliver the take-home message for a non-doctor audience (management, sales, IP):
• 16 million patients treated with aligners means a column of enamel with the height of 8000+ meters had been and continue to be unnecessarily sacrificed using IPR liberally, (8000m is the cruising altitude of a commercial airliner).
• 16 million patients treated means a column of composite with the height of roughly 385kms used for unnecessary attachments (that’s equivalent to low earth orbital altitude)
• A significant percentage of the 16 million patients suffered from unnecessary number of aligners and lengthy inefficient orthodontic therapy.
• A significant percentage of the 16 million patients suffered from adverse TMJ side-effects to Invisalign process.
• A significant portion of the 2Billion+ aligners your company shipped end up as unrecyclable plastic piling in landfills.
Eventually, I gave up on Company X, and I decided to fabricate in-house my entire aligner consumption. As we proceeded with in-house fabrication, we very quickly identified key areas of difference between my clinical aligner method, we call Biolign (Biologically Sensible Aligners) and that of Company-X, below is a high-level summary of my findings:
• I can deliver my precise class 2 medical device aka “aligner” same day or next day at the latest.
• I can have my patients’ work models printed at maximum resolution (50 microns to be specific)
• I can customize my patient’s aligner cutline to complement my clinical mechanics.
• I can optimize aligner efficiency (angular and linear velocities across all six vectors of movement), therefore optimizing my patients’ therapy.
• I can select the foil (plastic) materials for my patients.
• I can avoid attachments entirely.
• I can minimize IPR.
• I can readily avoid lateral open bite as a side effect of aligner therapy.
• I can readily avoid TMJ flareups as a side effect of aligner therapy.
• I can achieve +90% predictability on all vectors of movement.
• I can more readily manage variable compliance levels in my practice.
• Patients report better fit and esthetics of in-house aligners vs Company-X
As a biomechanics expert in orthodontics, I have exhausted ALL options to get Company X’s clinical and engineering teams to listen to my scientific and clinical feedback, they were made aware that I have evidence to prove that current levels of enamel filing prescribed is unjustified (as one example), this and many other points related to patient care have been relayed to management, engineering, and IP teams, all fell on deaf ears.
My conclusion, I do not think commercial outfits care about “evidence”!
VV (Vicki Vlaskalic) presents lectures sponsored by Align Technology
Dr Badawi, I sense your frustration and it is clear that you are passionate about improving this rapidly developing technology. Go for it !- competition can only benefit our profession. It appears from above that you have much data corroborating your appliance system. (I am not sure about the IPR comments – I simply leave the “IPR off” default on my prescription form and introduce it only if I deem it is required),
As for commercial outfits not caring about evidence, I am sure they do, especially when it is “marketable”. That’s the flip side, right? The innovations that they will likely introduce initially , in any such company, are those that may be more easily applied to existing workflow and manufacturing process. Routinely obtaining a high standard of treatment outcome whilst maintaining a high standard of dental health and patient satisfaction in significant number of patients will attract attention. Would love to discuss each point raised above but not sure if this is the place – will look out for your lectures. Thank-you.