Foot posture causes malocclusion!
Sometimes I come across papers that may seem to be just weird. This new paper looks at the association between foot posture and malocclusion.
The authors of this paper start by stating that functional disturbances of the masticatory muscles may be transmitted to other muscles along “muscle chains”. This may also be reversed and that the dental system may be influenced by imbalance in other areas of the body. They then suggest that early correction of malocclusion may minimise or eliminate the need for further treatment. As a result, we need to evaluate and correct foot posture early.
A team from Spain did this study. Medicine Journal published it.
Ana Marchena-Rodriguez et al.
Medicine: Doi http://dx.doi.org/10.1097/MD.0000000000010701
They did the study to answer this question;
“Is there a correlation between foot posture, footprint parameters and anteroposterior malocclusion”?
What did they do?
They did a cross sectional study of 189 6-9 years old children who they randomly selected from public schools in Malaga. They approached the parents of the children using a questionnaire that asked a range of questions about foot posture, breathing etc and these influenced the inclusion/exclusion criteria. These were extensive.
They then examined the children in their schools. They measured the following;
- Foot posture Index (FPI). This evaluates the nature of foot posture in 3 planes of space. An expert podiatrist measured this.
- The Clarke Angle. The expert podiatrist measured this from a tracing on a pedigraph.
- Angle’s classification: An orthodontist collected this data.
The orthodontist and the podiatrist were blinded to each others scores.
They chose the right foot only for the analysis and they measured association between the variables with the Pearson Correlation.
What did they find?
They found that 67% of the children had Class I, 21% Class II and 10% Class III molar relationships. They presented the data from the Clarke angle and FPI as parametric data and then did a non parametric test between the groups of Angle’s Classification (but this does not measure association). Here is the data as an imported table.
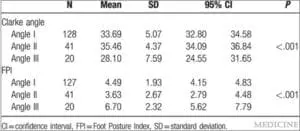
I looked up the normal values for FPI and in the child population this is 3.7 (SD=2.5). The values that they reported are within this range.
Their statistical analysis revealed that there was an association between the FPI, the Clarke Angle and dental classification. They then concluded;
“The Clarke angle decreased as the Angle classification increases from Class I to III, whereas the FPI is greater as the Angle Classification increases from Class I to III”.
This is an important statement as they suggest that the Angle Classification, which is a nominal scale, “increases”. This is an error because a nominal scale cannot increase.
In effect, I felt that their data presentation and statistical analysis was confusing and incorrect.
What did I think?
Over the last couple of years I have had many debates on this blog with the orthodontic “fringe”. I and others have consistently asked for evidence to underpin their theories. Some of the fringe practitioners flagged up and to be honest if this the best that can be done then there is no evidence to underpin the theories. This paper has the following major deficiencies;
- They do not provide sufficient details of the way that they selected the population of children
- The statistical analysis and data presentation is a complete muddle
- Association is not causation.
- The values of the FPI were within the range of a normal population.
- The use of Angle’s classification is a major error because this may be influenced by many co-founders, for example, missing teeth and dental caries. Unless foot posture influences caries!
- Importantly, the hypothesis that they were testing is not based on research data or even conventional wisdom. This is important because if we carry out a sufficiently large number of studies looking for something, then we will find it!
I know that my viewpoint will cause some discussion. Lets keep it scientific?
Finally, I have decided to review a few more of the “orthodontic fringe” papers over the summer. Next up is a paper by the London School of Orthotropics on the prevention of canine impaction with orthotropics.

Emeritus Professor of Orthodontics, University of Manchester, UK.
I can’t wait to read your next post.
Pardon the pun, a bad case of Hoof and Mouth Disease.
That you. Every once in a while it’s nice to see something light.
Hi Kevin:
It all depends on your definition of ‘weird’. I use a different definition of malocclusion (Brit Dent J 2007) that follows from my definition of occlusion, which states; The occlusion (or bite) is an end-point of the body with respect to the plantar surfaces of the feet, and within these two boundaries, all functional spaces for normal physiologic processes need to be accommodated. This definition emanates from the fact that enamel is derived from surface ectoderm, and it’s known that curvature during embryogenesis (reversal) leads to the rostral-most cranial ectoderm ending up in the mouth, for example as mucosa of the hard palate, detected using molecular markers/molecular biology techniques. Clinically, some dentists use oral orthotics to improve functional space for the TMJ. Similarly, podiatrists use foot orthotics working from the other end of the system. Some chiropractors and osteopaths are familiar with the idea of the ‘kinetic chain’ and work with it to address postural compensation. On the other hand, dentists/orthodontists work on (developmental craniofacial) compensation, most often in severe orthognathic surgery cases, but the principles apply to mild and moderate cases too. We did a couple of studies with our chiropractic colleagues on this topic. Remember, in the cranio-caudal axis, the next bone below the mandible is C1 and its horizontal axis of rotation is C1/C2. There are several papers in the orthodontic literature on this topic (Huggare et al).
References
Huggare J. Association between morphology of the first cervical vertebra, head posture, and craniofacial structures. Eur J Orthod. 1991;13(6):435-40
Singh GD. Outdated definition. Brit. Dent. J. 203(4), 174, 2007.
Chapman DC and Singh GD. Combined effect of a biomimetic oral appliance and atlas orthogonist cervical adjustment on leg lengths in adults. Annals Vert Sub Res. 46-50, 2013.
Singh GD and Chapman DC. Craniofacial changes after combined atlas-orthogonal and biomimetic oral appliance therapy. Annals Vert Sub Res. 4, 112-118, 2014.
I just read the paper, i totally agree with you, it doesn’t make sense to go from class II to class III without going through class I « the Clarke angle tends to decrease as Angle classification increases from Class I to III …………… »
To play the Devil’s advocate [I’m a man of wealth and taste!! 😉 ] and not having read the article but it would seem from Kevin’s clipped results that the authors have an incorrectly worded conclusion. The FPI ‘means’ do not increase from Class I to III but actually increase from Class II to I to Class III. Conversely, the Clarke’s angle decreases from Class II to I to III. However, there are still the other flaws as Kevin pointed out and no causal ‘association’ established but possibly a ‘relationship’ with Sheldon’s somatotypes? (I am laterally thinking out loud here – ‘have some sympathy…Use all your well-learned politesse’). Otherwise it seems to be the Podiatric version of Pont’s index.
A scientific discussion on this topic seems not to be possible since there appears to be no science to support, illustrate or deny the connection between the feet and the occlusion, so perhaps we can only rely on opinion and experience.
It is clear, as you say, that this study is not perfect in its design or execution, however it touches on the very real fact that the feet and the occlusion are closely connected through the intervening fascia and muscles, the bones acting merely as the links in the system. I know that it works because I have seen it function, in both directions. However, I very much doubt if any foot dysfunction could affect, or be affected by, the Angles classification. A cross-bite is perhaps more likely.
But for an orthodontist to be dismissive of the fact that the occlusion is a crucial component in body posture and balance is very worrying. Italian chiropractor Jean-Pierre Meersseman DC showed irrefutably many years ago that a patient’s tilted pelvis (indicated by scoliosis and a leg length discrepancy) could be corrected by correcting the occlusion, in at least 80% of cases.
We are all aware of Class II cases with a head-forwards posture; I know that if I do not wear my occlusal orthotic I will have low back pain in 24 hours. Conventional wisdom depends on where you are coming from!
Really? Irrefutable you say? As irrefutable as unicorn flatulence causing migraines? Or, succubi intrusions leading to insomnia?
Please enlighten the uninitiated masses about Jean-Pierre Meersseman’s study…was it adequately randomized with a control group, appropriate statistics etc.? Or is study design not relevant when one has such an incredibly ludicrous idea? We would like to know more about these theories that conflate fantasy and reality.
We are having some pediatric dentists who are recommending wholesale frenectomies (maxilla, mandible, labial, and lingual) for the prevention and correction of small arches and classII and Class III skeletal relationships. Is there any research to support any of this?
The relationship between occlusion and foot posture is significant, demonstrable, but I can’t agree with the author’s take on the results. For those who have used kinesiographs in the past, Zebris (German) made a unit that could integrate a foot pad, so that you could monitor postional and force/pressure changes in the foot posture, as changes to the occlusion were made. For example , if a patient had an occlusal cant, you might see an uneven weight distribution in the feet, placing an orthotic in the mouth to correct the cant would often result in an immediate postural change and rearrangement of the weight distribution in the feet. So the overall premise of the article makes sense if you believe that the skull/mandible complex sets at one end of the postural chain. If your world is occluso-centric, then I don’t know what you think. The nice thing about the Zebris unit is that the results are reproducible, and measurable,if you are applying being reproducible and measureable as conditions to a theory being accepted.
There have been other articles written about the postural relationships and occlusion. George White, former head of pedodontics at Tufts University, published a series of articles discussing the postural/occlusal relationships, and I do know that there are many others in the Chiropractic literature discussing the same thing.
I disagree with the article in that I believe that there is a top down relationship between occlusion and footposture and not the bottom up the author discusses.
I am prepared for some of the comments my post might elicit. However, the seeming hilarity of the article is not the primary focus but the presentation of the material should I believe in fact is valid, just IMO the conclusion is wrong.
This seems like one of those intentional propaganda techniques again: the effects of occlusion on the spine and body have long been known, so could you have deliberately misinterpreted causation/ deliberately titled your post to suggest the researchers have misinterpreted causation ‘foot posture causes malocclusion ‘ and pick out a bad (but not as bad as some ‘conventional’) research example possible simply to paint the ‘fringe’ in a bad light and then drop the bomb of orthotropics is up next while all you’re subscribers are salivating. Most people are reading this blog focusing on how bad fringe research must be, and no one has stopped to realise the obvious agenda here. A great way to set up your audience for the next blog, perhaps a career in politics is on the cards?
There is a reason the “fringe” is called that. Why would it ever need to be painted in a bad light given how bad it already is?
It’s precisely these sort of emotional responses that immediately and convincingly make the case against junk science.
Of course when one has no evidence, the next step (obviously!) is to level inept ad hominems at the other party instead of providing proof. So easy!
Perhaps a career in conspiracy theories is suitable for these self-nominated inquisitors of hidden “agendas”?
FAO Dr Keenan
I read your offensive remarks with a deal of sadness, because you are clearly one of those orthodontists with his head so firmly buried in the sand that you are quite unable to see or hear anything that is going on around you.
The Meersseman Test has been around for over 40 years, and has proved to be ‘irrefutable’ as well invaluable to me, using it almost daily during my last 10 years of practice. The principle being that if there was a connection between a patient’s malocclusion and their spinal/pelvic imbalance, the worst thing I could do would be to ‘fix’ the spinal issue in place by permanently (orthodontically or restoratively) altering the occlusion to conform to the imbalance.
But why on earth would one want a RCT to verify the existence of a normal body function? Should we have RCTs to verify a swallow pattern, opening our mouth, walking or touching our toes?
The Meersseman Test is just that, a test – harmless and totally non-invasive – to provide information on which way a spinal imbalance is being driven by ascending or descending influences. 20% are ascending and therefore have no connection with the occlusion. The Meersseman Test is not treatment; it is an indicator of possible treatment need and referral to a chiropractor or osteopath.
Whether you believe it or not, it still happens. If you really cannot believe there are functional links between the occlusion and the rest of the body, I suggest you have a chat with a friendly osteopath or chiropractor, or should we run an RCT first to be sure they are valid health care professionals?
Dr. Stimson – I have read many of your posts with a great deal of interest. You seem quick to take offense and umbrage instead of addressing the points. You are clearly not interested in facts and prefer to dwell in the land of self-concocted speculative fiction.
Where is the data supporting this link you speak of? I suggest you rethink how you apply ridiculous anecdotes to the question at hand. So according to you, we should just discard all science and just believe based on superficial claims? Osteopaths and chriropractors are the champions of fringe non-science as you have proven to be, time and time again. I suggest you depart from the land of absurdity and illogical thought and read about the scientific method.
Noel – Please provide citations or studies that prove your point. We cannot believe you just because you say something. This is a scientific specialty unlike chiro or osteopathic medicine. Perhaps your type of science would be more amenable to that type of ill-proven therapy. All your analogies are wasted in the absence of concrete evidence. Orthodontics should be past the point of believing gurus and other so-called “experts”.
There is definitely a link between foot mechanics and occlusion.
In a paper I published in 2013, I demonstrated radiographically that proprioceptive insoles change the frontal plane position of the cranial:
Rothbart BA 2013. Prescriptive Insoles and Dental Orthotics Change the Frontal Plane Position of the Atlas (C1), Mastoid, Malar, Temporal and Sphenoid Bones: A Preliminary Study. Journal of Cranio Manidibular and Sleep Practice, Vol 31(4):300-308.
Changing the frontal plane orientation of the maxilla will definite change the occlusion.
Professor Rothbart
Interesting. A viable scientific hypothesis would be that this is related to hormonal changes due to obesity that often affects that angle.