Bone anchored Class II treatment: Is this possible or necessary?
Functional appliances are a well established method of Class II correction, but they do have problems. Is using miniplates to deliver Class II force a treatment method?
Functional appliances are a relatively effective method of treating Class II occlusion. The effectiveness of this has been studied in many trials and systematic reviews. After all this research I feel that this area is not as controversial as some people suggest. However, these investigators outline a new technique of correcting Class II problems using mini-plates screwed into the maxilla and mandible. They make real claims for the effectiveness of this treatment and so I have looked at this paper very carefully.
Abdullsalam Abdulqawi Al-Dumaini et al.
Am J Orthod Dentofacial Orthop 2018;153:239-47
https://doi.org/10.1016/j.ajodo.2017.06.020
A team from Syria and Yemen did this study.
The authors declared a conflict of interest as some of them have patented this technique.
What did they ask?
They did a study to ask
“What is the effect of correcting Class II malocclusion with miniplate supported Class II force”?
What did they do?
They carried out a prospective cohort study. The PICO was
Participants: 10-13 year old patients with skeletal Class II malocclusion
Intervention: Treatment with skeletal anchorage Class II mechanics
Comparator: An untreated control group. No details were given in this paper.
Outcome: Multiple cephalometric measures
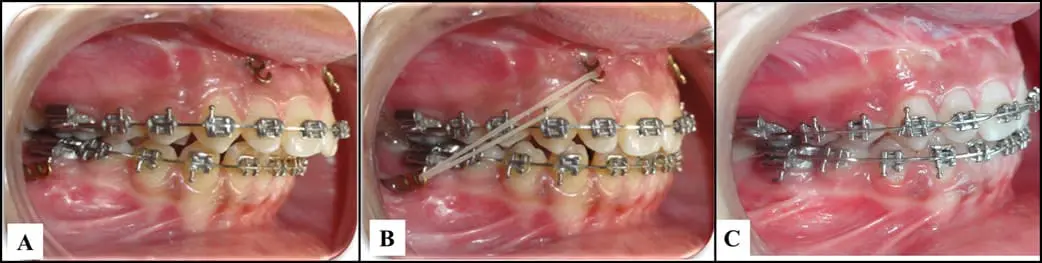
They used MBT prescription appliances to align and level the arches. They then fixed orthopedic miniplates to the mandible and maxilla under LA. 28 days later they loaded the miniplates with 250g elastic force for 3 weeks, then 350g for 3 weeks and finally used 450g per side for the rest of the functional phase.
![]()
They collected cephalometric data after alignment and levelling with fixed appliances and after they had reduced the overjet to 1-3 mm. They compared 23 ceph measurements with “t” tests.
What did they find?
They did a cephalometric study in which they compared many related measures with univariate statistics. This means that there is a high chance of false positive findings occurring by chance. We need to bear this in mind when we look at the data.
Firstly, when they compared the treatment group to the untreated control it appeared that 10 out of the 20 measurements were significantly different. I am not going to go through all these, however, SNB was 2 degrees greater in the control group. They then compared the changes within the two groups and every measurement was different. They also evaluated the changes within the two groups and again nearly everything was statistically significant, but the effect sizes were small.
The authors concluded that:
“Bimaxillary miniplate anchorage promotes the correction of skeletal Class II malocclusion mainly through skeletal change”.
What did I think?
Firstly, I think that this study had the potential to be a really good cohort study that could lead to the possible further development of this technique and the authors should be congratulated on doing this work.
However, one of the reasons that I write this blog is to help interpret the results of studies that are published in the literature. I, generally, try to be constructive. I also attempt to be objective and not be over critical. However, when I have looked at this study I am not sure that I agree with the conclusion.
I have two main concerns. The first is with the choice of the control group. The authors do not give any details of how this group was selected. The only reference is to a thesis, and I could not get a copy. Furthermore, there were many differences between the control and the treatment group before treatment. Secondly, they have analysed many cephalometric measures in several ways and then picked their choice of important variables to discuss. I think that this has led me to find it difficult to identify how they reached their conclusion.
I would also have liked to see some information on the patients perceptions of their appliances. This is an important outcome that should be considered, particularly, for treatments that are invasive.
I cannot help feeling that this paper would be better if it was a simple cohort study without a control group, and I wonder whey the AJO-DDO referees did not suggest this?
Finally, I shall stick with the Twin Block for Class II correction. Research shows that it works and it is not as traumatic as placing bone anchored miniplates. But, it would be great to see more research on this technique, as it may be a good step forwards.

Emeritus Professor of Orthodontics, University of Manchester, UK.
Thanks for this very interesting Blogpost.
My first thought when I read the above mentioned article was:“How can an invasive (possibly non-compliance?) technique (like miniplates) be combined with elastics (highly compliance depended technique)…? And how has the compliance been measured…?“
What are your thoughts about this?
Thanks very much!
Best regards
You make a good point. I would have liked to see this treatment compared to treatment as usual, which could be another functional appliance. We could also have outcome measures of compliance, patient acceptance etc. Again, I am surprised that AJO referees did not suggest this. It is time for us to move away from searching for skeletal change..
I find the choice of control group quite odd. Its like running a cancer treatment trial and having the control as no treatment !!
Yes, I agree, but their question was looking at skeletal changes and to evaluate this they would need the untreated control group. However, they did not provide any information on this group. Also, see my other comment on choice of control or treatment as usual
My first thought was “what is this technique doing to the cranio-facial bones?” Unfortunately, many dentists are unfamiliar with the reality that the cranial bones have inherent mobility and flexibility; if the elastics employed can apply sufficient force to move the masticatory structures into a new relationship, they will inevitably have a considerable effect on the facial and cranial bones.
As described, this will result in the maxilla being pulled back into the skull as well as bringing the mandible forward (the law of equal and opposite forces).
One has to wonder if the cephalometric assessments compared pre- and post-treatment positions of the maxillae.
The stated objective of the study seems to be the reduction of the overjet as efficiently as possible, compared with a (mythical) control group. Since overjet is probably the least important health risk within orthodontics, I think it is sad that this study’s workers did not use, or at least include, a more significant yardstick such as airway change.
We need to remember that malocclusion is not the problem, but the result of the problem, and that an increased overjet is a result of the malocclusion. Treating the results themselves alone without addressing the underlying cause is to invite relapse.
I always enjoy reading your blog.
Thank you for your valuable contribution to the profession.
As far as this particular topic, I am curious why you mention preferring use of the twin block over an approach that is less dependent on cooperation such as the Forsus.
Thanks for the comments. I suppose that my choice of functional appliance is down to my personal preference, as research seems to show that the choice of appliance does not influence outcome. I have tried using Herbst appliances but stopped because of breakages and I have tended to stick with the Twin Block ever since..
Very informative post! I always enjoy reading your blog.Thank you for your valuable contribution to the profession. They will learn a lot.
orthodonotic foster city