A simple trial of the extraction of primary canines to intercept palatally displaced canines provides us with great information.
It is common practice to remove primary canines to intercept palatally displaced canines. This new paper provides us with great guidance on when this is likely to work or not…
I have posted about this treatment before and I concluded that the evidence underpinning this procedure was limited. Fortunately, a really good trial of this treatment was done and I posted about this here. The authors have done a follow up to identify whether panoramic radiographs can predict the chances of successful eruption of a PDC. I thought that this study was great. A team based in Gothenburg did the study and the EJO published the paper.
Julia Naoumova and Heidrun Kjellberg
European Journal of Orthodontics, 2018, 1–10 doi:10.1093/ejo/cjy002
The paper is not open access, which is a shame.
In their introduction the authors pointed out that they had looked at the predictive effect of CBCT views in an earlier paper. However, the use of CBCT is not widespread. As a result, they wanted to look at the predictive power of panoramic radiographs (PAN) to identify those PDCs that may erupt with or without the extraction of the primary canine.
They wanted to answer this question.
“Are there any possible predictors and cut-off points that we can identify on a panoramic radiograph to find out whether extraction of the primary canine is beneficial in children with a PDC’?
What did they do?
They did a RCT with a 1:1 allocation. The PICO was
Participants: Children aged 10-13 years with maxillary unilateral or bilaterally PDCs. Importantly, they did not have crowding greater than 2mm (I shall return to this later).
Intervention: Extraction of the primary canine
Control: Non extraction of the primary canine
Outcome: Eruption of the canine at 12 months.
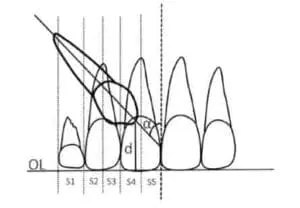
They assessed the initial position of the PDC on the PAN using the method first described by Ericson and Kurol. They based this around the following measurements.
Alpha angle: The angle formed by the long axix of the canine and the midline
D: The distance in mm from the canine tip to the occlusal plane
Sector: The mesiodistal crown position in sector 1-5. I have pasted in their diagram here.
They developed logistic regression models to determine cut-off points for successul and unsuccessful outcomes. They also used a Receiver Operating Characterstic (ROC) to calculate the predictive power of the test. I thought that these methods were complex and very appropriate.
Information on the success rate etc of removal of the primary canines was included in their earlier paper and in this earlier blog post. Essentially, they showed that removing the primary canine was an effective measure.
What did they find in this study?
I thought that it was really interesting that they found the following:
The extraction of the primary canine was the baseline variable that most effected the eruption of the PDC. This was followed by the alpha angle, the sector measurement and the age of the patient.
They concluded the following:
- Interceptive extraction is most likely to be of benefit when the alpha angles is 20-30 degrees and the PDC is located in sector 2-3.
- Simple observation (non extraction of the primary canine) is likely to be successful for patients with PDCs with an alpha angle of less than 20 degrees in sector 2.
- When the alpha angle is more than 30 degrees and located in sector 4, it likely that interceptive extraction will not be effective. That is, we may as well get on with exposure and alignment, if this is indicated.
What did I think?
I have always thought that this was a great small trial that answered a very clinically relevant question. They did a good randomisation, concealment and allocation. I have a slight concern about the blinding in the earlier study, but this is not relevant to this part of the study because the pre-treatment radiographs were blinded.
A major limitation of the study is that they only included cases with good pre-treatment alignment. I am not sure why they did this. I feel that this is important because it means that the findings are only relevant to children with PDCs with well aligned arches.
However, these comments are minor and I think that overall this paper provides us with great clinically useful information.

Emeritus Professor of Orthodontics, University of Manchester, UK.
Great post. It agrees with studies of Baccetti, Kurol, and other authors. Thank you for sharing.
I like this – there seems to be some objectivity in making the decision– do we actually have odds/probability of how much difference any of these interventions will (or won’t) make?
Stephen Murray
Swords Orthodontics
Again, like your previous blog mentioned, I note that it could also be that extraction of the Cs may accelerate the eruption of the palatal U3s. It would be interesting to know what happens for the nonextraction group in the period that follows if it is without intervention as to whether the significance decreases over time. I also look forward to a follow-up study that applies these guidelines to another study sample group to test them. Truly a shame it is not open access.
Respected Dr Kevin O’ Brien,
Thanks for sharing with us all great studies always. Hats off to your commitment towards Healthy ,clean Orthodontics.
Regards,
Dr Rajesh J Kamdar.
Nice article. Good study design.
Early interception of palataly displaced canine with crowding not more than 2 mm and no placement of fixed orthodontic appliances ( might upright the root of upper latral incisor and worsen the eruption path of the permanent canine.) in my opinion is a good interceptive orthodontics practice . In this treatment philosophy the dental development was enhanced in less cost and less chair side time.
Dear Dr. O’Brien,
Thanks a lot for sharing this study and making the results available for everyone as well as for all your blogging activity. However, I want to stress on two relevant points:
1. I feel that the selected age group (10-13 yrs) is a bit below the age that parents could seek consultation for what seems to be a dental problem and that General Dentists could worry enough to refer to an Orthodontist.
2. There is nothing mentioned in the study that describes the status of the primary canine (presence or abcense of root resorption) which could give valuable information about the cause of permenant canine palatal displacement .
Kind Regards
Thank you for posting this! I think most orthodontists totally agree, but it’s great guidelines for GP’s as to when to refer.
I don’t think many GP’s are comfortable with exposure surgery cases.
I’ll be sharing this with many docs today- appreciate it!
Kevin O’Brien. Did this study you have reviewed give you any indication of the cause of PDC and how extraction of the primary canine helps address whatever underlying issues led to PDC and might thus lead to other problems in the future if unknown and unchecked?
Dear Prof o’ Brien
the post is very interesting, but several important works(Effect of interceptive extraction of deciduous canine on palatally displaced
maxillary canine:
A prospective randomized controlled study
Farhan Bazargania; Anders Magnusonb; Bertil Lennartsson) shows that if you associate a space maintainer to the extraction primary canine the success of PDC increases significantly.
What do you think about it? From the clinical point of view you use a Nance or Goshgarian to increase the chances of PDC eruption ?It could be an overtreatment?
This may seem a stupid question but could I ask if the extraction are carried out using a local or general anaesthetic . As today we have discovered our daughter has to have this procedure.
Hi you can have extractions done under local or general anaesthetic. Your dentist will be able to discuss this with you.