Maxillary expansion improves children’s quality of life! A tremendous new trial.
Now and then, a team of investigators publishes an excellent paper. This new report outlines a trial that provides us with clinically important information on the effects of RPE.
Many investigators have researched the effects of maxillary expansion. While these trials have added to our knowledge, they have tended to concentrate on the morphological impact of treatment. These may not be relevant to our patients. Therefore, I thought it was great to come across this paper reporting a trial that looked at oral health-related quality of life.
The study team pointed out that posterior crossbites due to maxillary constriction may lead to problems with function, altered masticatory patterns, and increased airway resistance. These factors are likely to influence oral health-related quality of life. As a result, it is logical to do a trial looking at the effect of treatment on quality of life.
A team from Brazil did this trial. The AJO-DDO published the paper.
Matheus Pithon et al. AJO-DDO in presss. https://doi.org/10.1016/j.ajodo.2021.08.015
What did they ask?
They asked this simple question
“Was there any effect of the treatment of maxillary deficiency using RPE on self-perceived Oral Health Quality of Life (OHRQOL) of children”.
What did they do?
They did a two-arm parallel randomized controlled trial with a 1:1 allocation. The PICO was
Participants: Children aged 8-10 years old with transverse maxillary deficiency and bilateral posterior crossbite.
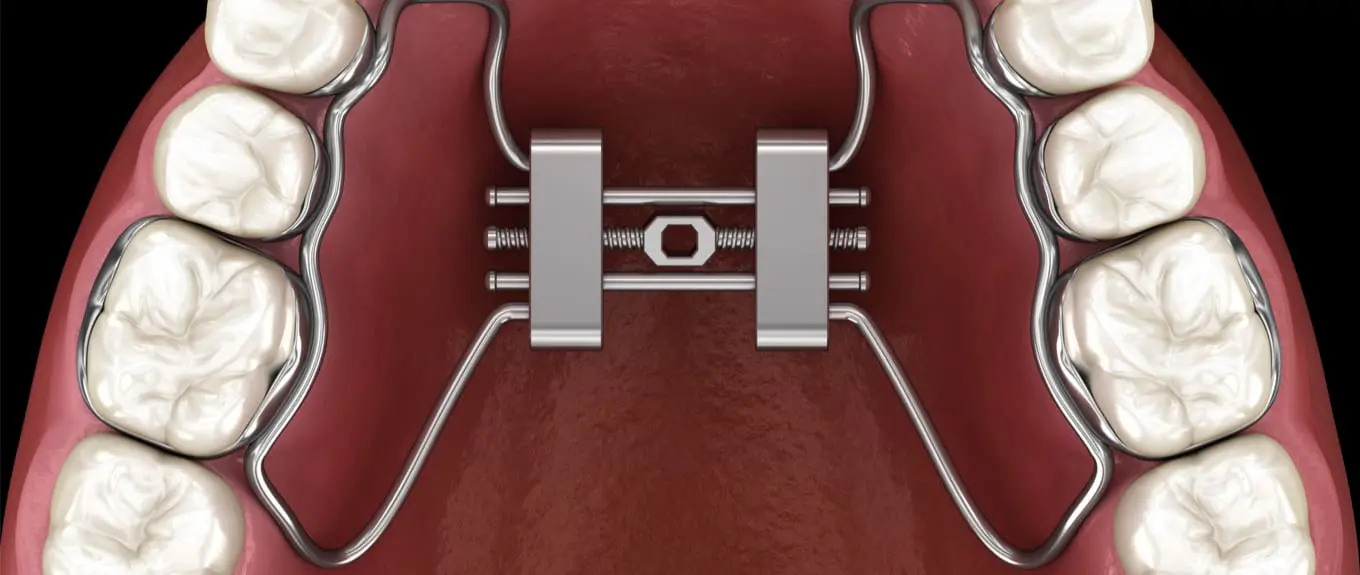
Intervention: Rapid palatal expansion with a hyrax expander.
Control: No treatment
Outcome: Oral health-related quality of life using the Child Perception Questionnaire. This is a validated instrument that investigators have used in orthodontic studies.
They did a nice sample size calculation, used pre-prepared randomization, and concealed the allocation using sealed envelopes.
They collected the data at the start of the study, after two weeks of RPE, at the end of RPE, and one month after removing the RME appliance. This period tended to be seven months of treatment.
The team set out to randomize 40 patients to each group. They were not blinded to treatment allocation. Finally, they used relevant complex statistics.
What did they find?
All the participants completed the study. Importantly, there were no differences between the groups at baseline.
When the investigators looked at the results, they found that OHRQOL scores increased by 17%. This meant that OHRQOL was reduced. However, at the end of treatment, PHRQOL significantly improved (72% reduction). Importantly, they found this for all the domains of oral symptoms (70% reduction), functional limitations (90% reduction), emotional well-being (89% reduction) and social well-being (42%). These differences were clinically and statistically significant.
The authors concluded:
“Correction of the maxillary transverse maxillary deficiency by RPE in children aged 8-10 years improves OHRQOL. However, there is a temporary worsening of OHRQOL during the treatment of this condition using RME”.
What did I think?
This trial was an excellent study that had been carried out and reported well. The findings are clinically useful and emphasize the treatment effects of an intervention relevant to our patients.
Occasionally, I have been accused of not being positivite about some of the studies that I discuss. While I accept this criticism, I try to be objective and point out issues we need to consider when interpreting papers. As is my usual practice, I looked very closely at this paper, and I feel that this is study is excellent. Some may want to see the morphological effects of the treatment. However, this is not relevant because the critical outcome is the patient’s perceptions.
Finally, I think that this paper should be widely read and quoted. It should reinforce our practice.

Emeritus Professor of Orthodontics, University of Manchester, UK.
How did they differentiate on quality of life factors between the effect of just removing the RPE- appliance which itself affects all these factors
and believed treatment effect? I have not read the article itself, yet- my question is based only on your blog.
Exactly right.
In acupuncture trials, they use sham acupuncture as a control and find no treatment affects. This is in contrast to the results obtained when a “no treatment” control group is used.
I remember a radio interview, in which an Intensivist promoted the benefits of acupuncture for pain, as she said that she saw positive results in ER every day. The reporter asked what treatment untreated group received? He was told that they were left in the waiting room and were not given attention unlike the treatment group that were moved to a warm room and were given attention for their concerns. At least the reporter had a skeptical inquiring mind, so essential for scientific reasoning.
One month after removing the intrusive device is also hardly enough time for the emotional effects of treatment to dissipate.
I remain skeptical, as I do about the many biased studies done by McNamara on expansion.
Could this just be a post treatment bounce from having the appliance removed?
1 month is not a long time re follow up.
Thanks for another very useful review. These are remarkably interesting findings. No doubt the “airway friendly orthodontic cults” will shout these results from their collective roof-tops. Caution advised that these participants: children aged 8-10 years old presented with transverse maxillary deficiency INCLUDING bilateral posterior cross-bites. For many years of clinical practice, I expanded substantial numbers of children who did not present with posterior cross-bites. Using a Boley gauge and standardized reference points I measured and waited for the lower arch to “passively” expand. The expansion device remained passively in place. Retention time ranged from 6 – 9 months holding ideal “over-expansion”. The passive lower arch expansion response did not occur. Rather, excess buccal overate remained until after the expansion device was removed. Allowing that arch coordination (ideal buccal overjet) is desirable, I remain curious as to how the patient’s dental arches will coordinate to ideal buccal overjet if maxillary expansion is undertaken in the absence of posterior cross-bites.
Hello Gerry
To your question, ‘….I remain curious as to how the patient’s dental arches will coordinate to ideal buccal overjet if maxillary expansion is undertaken in the absence of posterior cross-bites.’, Jim McNamara stated in his classic 2000 AJO/DO paper honoring Dr. Tom Graber, ‘Maxillary Transverse Deficiency’ (https://www.ajodo.org/article/S0889-5406(00)70202-2/fulltext), ‘Further, I am impressed with the treatment effects produced by rapid maxillary expansion (RME) in patients without crossbite. Orthodontists traditionally have used RME to correct crossbites, but little else. In contrast to the aggressive approaches often taken in treating skeletally based anteroposterior and vertical
problems, many orthodontists have been reluctant to change arch dimensions transversely. Yet, the transverse dimension of the maxilla may be the most adaptable of all the regions of the craniofacial complex. It is my opinion that many, if not most, transverse skeletal imbalances in the maxilla are ignored or simply not recognized, and thus the treatment options for such patients of necessity are more limited than if these
imbalances were recognized. Let me explain further. Other than crossbite, two of the most common problems encountered by the orthodontist are crowding and protrusion of the teeth, both of which derive from discrepancies between the size of the teeth and the size of the bony bases. Howe et al4 have shown that dental crowding, at least in individuals of European ancestry, appears to be related more to a deficiency in arch perimeter than to teeth that are too large…..’. Dr. McNamara goes on, ‘Counterintuitively, certain Class II malocclusions also may be associated with maxillary deficiency. From a sagittal perspective, maxillary skeletal protrusion occurs only in about 10% to 15% of Class II patients, whereas as many as 30% of Class II patients may have maxillary skeletal retrusion, often associated with an obtuse nasolabial angle and a steep mandibular plane angle.9. In this article Dr. M also discusses the relatively high proportion of class II’s as having a co-morbid transverse deficiency (‘It is my opinion that most Class II malocclusions in mixed dentition patients are associated with maxillary constriction.’). JM also mentions his observation in his own patients that there is often ‘spontaneous correction’ of some class II pts. who are retained in maxillary over-expansion. McNamara and others now, as is the case with the Brazilian study reviewed here, have acknowledged improved nasal airway health and overall HRQOL after maxillary expansion (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4596248/pdf/40510_2015_Article_105.pdf). One question for you sir, if RPE for the 8-10 year olds within this Brazilian cohort had been treated earlier, say whilst still in their primary dentitions (i.e., when their Dx of MTD was absolutely first discernible regardless of cross-bite presence or not yet), do you think it would’ve been medically-defensible, from a prophylactic point of view….in terms of malocclusion alone, not to mention other potential HRQOL factors, to go ahead and address the MTD at such a young age….and specially you Gerry, as a dual-trained ortho-pedo with with excellent behavior guidance training skills and experience?
Very interesting paper; but we need to resist the urge to generalize these results to children without transverse deficiency and posterior crossbite. This paper should not be used as an excuse to expand every child that walks through our doors.
Agreed
Dear Dr Riolo
Not only do I agree with you that this particular paper ‘…should not be used as an excuse to expand every child that walks through our doors.’, absolutely no paper should attempt to defend such an indefensible and deplorable practice. And that said sir, I also think it was not medically-defensible for any Institutional Review Board (IRB) to approve a protocol that stipulated withholding of a known therapeutic intervention (RPE Tx and improved naso-respiratory competence has been discussed within the med-dent literature for over a century…..references upon request) from an age-matched (8-10 yr olds) and disease-matched (Dx:MTD w/breathing disorder co-morbidity) cohort merely for the purpose of establishing a robust control group for statistical significance purposes (or not), is both short-sighted I think, and also unethical btw (read about how current IRB protocols in US and elsewhere had evolved from Nuremberg Trials records post WW II).
Perhaps a control with the same expansion device not being expanded. (Activated as a faux ratchet, rotate clockwise in the morning counter-clockwise in the evening).
Eliminate the euphoria from this obtrusive appliance being removed as the reason for the OHRQOL score changes.
The main reason for expanding the maxilla in the past was due to a constriction of the maxilla, due to a posterior crossbite, but today the main justification is for the health of the airways and the quality of life that derives from the latter assumption.
However, the only one qualified to determine the health of the airways is the ENT, we cannot invade lands that do not correspond to us, that is usurpation of functions, it is professional usurpation.
Only the ENT can do a Dx in this field and together with the sleep specialist determine if there is an abnormal function.
It seems that expanding the maxilla to make the nostrils more permeable is not very intelligent, since the main causes of airflow resistance are alterations in the airways themselves, such as allergies, adenoids, deviated septum, etc.
In addition, expanding the palate and thus expecting an increase in the volume of the nostrils does not guarantee that there is a better air flow, how much do we need to increase the volume of the nostrils for this purpose? And although the nasal volume improves, the air resistance occurs in the most posterior part, in the pharyngeal air.
This area is the one of clinical interest because in this area the collapse that causes sleep disorders and a whole cascade of alterations that affect the development of the child occurs.
Suspicions had been made about it for a long time, since then it has been questioned that having an open mouth does not mean having blocked airways, and that the patient is an oral respirator.
This topic is very controversial and will continue to give a lot to talk about for a long time.
I’d like for Prof O’Brien to elaborate upon why he’d concluded that, ‘….The findings are clinically useful and emphasize the treatment effects of an intervention relevant to our patients.’, and also, why he’d recommended, ‘…I think that this paper should be widely read and quoted. It should reinforce our practice.’.
Thanks, I made this comment because I thought that it was a nice trial that reported on outcomes that are relevant to our patients. I hope that this answers your question.
i think the paper needs read with caution (i don’t have full access) but it would appear they are claiming an improvement in OHRQOL by using RME to correct a crossbite, but the control had no appliance, so maybe it is the fact the child was being given additional attention was the important factor. The period was very short and I think concerns are right to be raised as we know the ‘Hawthorn effect’ and to me this may be what is being seen….
I would suggest a read of the paper by Oral Health-related Quality of Life, What, Why, How, and Future Implications by Sischo and Broder ; J Dent Res. 2011 Nov; 90: 1264–127 to help place things in context when reading QHRQOL based research and that in children when assessing OHRQOLti asses both parents and children