A new randomised trial of miniscrew supported RME
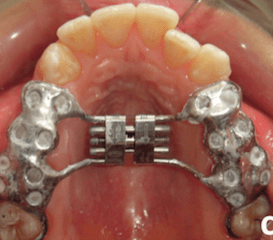
Rapid maxillary expansion (RME) is an important orthodontic treatment method. A recent development has been miniscrew supported RME. This new trial compares mini screw with tooth borne RME.
Traditionally, RME devices are placed directly onto the teeth. It has been suggested that this method does not always achieve maximum skeletal expansion because of tipping the molar teeth. Recently, bone borne expansion devices have been developed with the aim of reducing these drawbacks.
A team from Turkey did this study to compare tooth borne and bone borne RME devices. The Angle orthodontist published the paper.
Tugce Celenk-Koca et al
Angle Orthodontist: Advanced access: DOI: 10.2319/011518-42.1
What did they ask?
The asked whether there were any differences between conventional and miniscrews supported RME devices.
What did they do?
They carried out a two arm parallel randomised trial with a 1:1 allocation of interventions. The PICO was
Participants: Orthodontic patients requiring 8mm expansion with a mean age of 13.8 years (SD=1.2)
Intervention: RME supported by mini screws
Control: RME placed on the molars and premolars
Outcome: The primary outcome was correction of crossbite. The secondary outcomes were skeletal and dental measurements (including root resorption) from CBCT images taken at the start of expansion (T1) and 6 months later (T2).
They did a pre prepared randomisation and concealed the allocation using sealed envelopes. They carried out simple univariate statistics.
What did they find?
The groups were similar at the start of treatment. They randomly allocated both interventions to 21 patients in each group. Unfortunately, I could not find any data on whether the crossbites were corrected. I have extracted this data from their CBCT information and calculated the confidence intervals. I have only presented this for data collected at T2 because this provides us with sufficient information on the effect size
| Conventional | Bone borne | Difference | |
| Incisive foramen width | 4.7 | 6.7 | 1.9 (1.19-2.6) |
| Sutural width at premolars | 2.5 | 4.6 | 2.1 (1.4-2.7) |
| Sutural width at molars | 2.0 | 3.9 | 1.9 (1.2-2.5) |
When they looked at the buccolingual inclination of the teeth they found:
| Conventional | Bone borne | Difference | |
| Premolar | 87.7 | 92.1 | 4.4 (0.8-7.9) |
| Molar | 94.8 | 101.4 | 6.6 (3.6-9.5) |
There were no marked differences in root resorption.
The authors interpreted their findings and concluded;
“bone borne expansion increased the maxillary suture opening more than 2.5 times tooth borne expansion”.
What did I think?
I thought that this was an interesting study. Nevertheless, there were some areas that they did not clearly report. For example, the inclusion criteria was that the patients had to have maxillary restriction. I could not find any information on how they diagnosed this feature. They also did not report their primary outcome.
It was a shame that this was another paper that the Angle published that did not conform to the CONSORT guidelines for reporting of trials. I felt that this made it difficult to read and interpret. Perhaps the Editor will address this problem?
When I looked at the conclusions, I was concerned that they stated that bone borne expansion was 2.5 times the treatment effect of tooth borne expansion. Again, I could not work out how they calculated this effect. We also need to remember that expressing treatment differences in this way tends to over exaggerate the treatment effect.
However, we need to look at the effect size of the sutural expansion. This is only 2.1 mm and the CI suggests that it could just as easily be 1.4 or 2.7mm. The headline now is:
“bone borne expansion is 2.1 mm more effective than tooth borne”.
This does not sound so good. But you may think that this is clinically significant and is sufficient for you to adopt bone borne expansion. But we also need to consider whether the additional trauma and burden of care is justified by a difference in expansion of 2mm. However, this study allows us to give this information to our patients. They can then decide on their treatment method.
I am sorry to be so critical of a study that appeared to be well done, but we need to consider these issues when we interpret papers.

Emeritus Professor of Orthodontics, University of Manchester, UK.
 Evaluation of miniscrew-supported rapid maxillary expansion in adolescents: A prospective randomized clinical trial
Evaluation of miniscrew-supported rapid maxillary expansion in adolescents: A prospective randomized clinical trial
You don´t have to be so sorry to be so critical. I´m very thankful that you share your opinion/study with us. Your ” interpretation” of results is very useful for many people, like me.
I used to use quite a bit of tooth borne RME using cast silver splints very similar to those illustrated, made in the laboratory at Morriston Hospital, Swansea, Wales.
That this study found more expansion with bone rather than tooth supported expansion does not surprise me. I expect that the explanation lies as much in the elasticity of the periodontal ligament as in tooth movement through bone. I’m pleased that no difference in tooth resorption rate was found.
Surely, to obtain the same amount of expansion, one simply needs to activate the expansion screw a couple of mm further if the appliance uses the simpler tooth borne approach; which I submit is more readily acceptable to patients than mini-screws. (Though acceptance of mini-screw anchorage is seldom a problem).
Dear Dr. Howells, I agree with you and Dr. O’ Brien that the amount of expansion depends on the amount of activation and elasticity of the midpalate suture and design of the device is less important. Anyway, sometimes papers are very enthusiastic in reinforcing what they think. It is very difficult to compare the boneborn RME and the toothborne one because of the multiple variables that should be considered. The boneborn device does not compromise teeth and that is the main issue.And patients are getting more and more used to this aproach. And this devices are more esthetic , comfortable and allow placing brackets sooner. I really like them. Thank you for this exchange of opinions. Keep on with your blog Dr. O’ Brien
Thank you sharing us these valuable inforamations! You comment means a lot to us!
Yet again the issue here when trying to move bones around is “is it sustainable?”. Correct me if wrong but is there not evidence that the boney changes achieved by RME relapse, leaving the posterior teeth tipped outwards (assuming the tooth position is retained)?
You’re of course right that 2.1mm more expansion does not sound too impressive, even less so if you call it 1mm a side.
What about the age of the sample. The idea of using bone born is also to widen the limits related to age expanding in young adults/ adults. So info about age makes difference in particular also 2mm make the difference while expanding in young adults.
Dear Alessandro, I don’t think that boneborn RME is a substitute of SARPE. Only in borderline cases. At least my experience with elder patients with closed sutures was bad. And relapse is the other problem. Thank you for the exchange
I think this is an important topic that IMHO needs to be brought to to date. For example, sutures are not inanimate objects that can be “opened or closed”. I also wonder if they can be “expanded” since they have biologic behaviors. For example, craniofacial sutures, like any other biological system in the body, are subject to homeostasis. If these sutures that were “expanded” by 2.1mm are re-measured at, say 12 months post-treatment, I daresay their width will vary between 100-400microns or 250microns on average (0.25mm), which is about the same as the periodontal space on a periapical radiograph (and about the same width as cranial sutures). This phenomenon is encapsulated by the term ‘sutural homeostasis’. Comments like “elasticity of the periodontal ligament as in tooth movement through bone” make me smile. It is known that the periodontal “ligament” is likely not a ligament; it’s best described as a periodontal suture IMHO, since it’s subject to sutural homeostasis. The periodontal “ligament” does Not show elasticity. It’s behaves as a visco-elastic medium due in part to the properties of its extracellular matrix (which confirm that it’s not a ‘ligament’). The notion of ‘moving teeth thru bone’ is unlikely to occur in vivo IMHO, partly due to the phenomenon of sutural homeostasis. However, this biologic control mechanism can easily be overpowered by orthodontic forces to yield dehiscence, fenestrations, etc. We know that some children treated with RME don’t recover from this bone loss (and as adults are predisposed to periodontal bone loss). I wonder whether the ‘tooth-borne’ RME were tested for this unwanted side-effect?
Your aproach is very interesting Professor Singh. Do you this that slowing activation would be less harmful for patients ?
Thank you so much
I’ve noticed that Dr. O’Brien often criticizes researchers for leaving out data in their articles and it’s true that often these articles seem to have some holes in the write-ups. I’d like to point out, as someone who has once experienced having research published in a prominent orthodontic journal, that a limiting factor is often the word limit placed on articles accepted for publication. I understand no one will read articles that are too long-winded, but several journals require authors to edit their writing so drastically that it is inevitable that relevant information will be cut out.
For the study here, the major outcome I am interested in when comparing tooth-borne vs. bone-borne expanders is how the incidence of root dehiscences in the buccal plate compare and whether there is more bodily movement rather than tipping in bone-borne expanders. The summary in this blog barely mentions this, but I went to the original article and found the following:
“Decreased buccal bone and bony dehiscence are commonly documented as a result of RME due to osteoclastic resorption as teeth move through the buccal plate.3,7,22,23 The current results indicated that changes in the buccal bone occurred significantly less frequently in the miniscrew-supported appliance group than in the tooth-borne group. Considering the error study, it could be concluded that the buccal bone widths remained virtually stable in the bone-borne group. As previous reports already hypothesized, the differences between the two groups were most likely due to the absence of direct force application to the tooth crowns in the miniscrew-supported RME group.”
and
“In the current study, tipping of the maxillary first molars in the bone-borne RME group was significantly reduced in comparison with the conventional RME group. The decrease in the amount of buccal tipping of first molars is consistent with previous bone-borne expansion studies.20,21 Also, maxillary first premolars and first molars were uprighted by a mean of 0.6 8 and 1.38, respectively. Uprighting of the maxillary first premolars and first molars could be explained by the absence of a buccal force acting on the crowns and increased apical separation of the maxillary suture in the miniscrewsupported RME group, leading to a more upright crown inclination relative to the nasal floor. “
Thank you alot for sharing us this valuable information
While you make the comment that 2 mm. of lateral development of the nasal airway doesn’t seem significant enough to make much difference, from a flow standpoint with regard to nasal airway patency, that lateral difference is very significant. The increase in area and volume of the nasal passages is substantial, even with 2mm of total lateral increase. The studies on Sleep Disturbed Breathing from Stanford, especially those involving Dr. Christian Guilleminault, state that OSA in children who are not obese (and even in many that are) is a craniofacial structural problem. The research from this same and other sources also states that resolution of OSA and related disturbed breathing issues is primarily dependent upon achieving good nasal breathing, both at night and during the day, and that without that, the OSA, UARS, RERAs, etc., can’t be eliminated. In my experience, that amount of lateral nasal airway develoment is the difference, among other things, between sickness and health, between normal cognitive development and diminished cognitive capacity, betweeen normal behavior and various behavioral issues, including misdiagnosis of ADHD, etc.
The comment from Dr.Lipskis is borne out by my experience .This is an important and often,overlooked issue .
I think the ENT community would really benefit from an understanding of this -allergists also ?
I live in hope of my local ENT,s being more aware of orthodontic issues !
Always ,a great blog,
Dr Thompson:
I am presenting my findings on this topic at the ENT 2018 conference in London, UK in October – and at the Otolaryngology 2018 conference in Dallas, USA in November.
”I could not find any information on how they diagnosed this feature.”Kevin O’brien…
I think ….I find it in cephalometric analysis…more precisely… years ago Ricketts had found it …but he made a wrong comment …40. Cranial Deflection
High values may indicate abnormal mandibular growth…. wrong , because it shows skeletal maxillary narrow ….in lateral cephalometric analysis.
Unfortunately the authors don’t appear to report the number of turns or days ‘per group’ and only the overall average so the number of turns per group (amount of appliance expansion) is unclear. Therefore I feel the miniscrew (TAD) supported expansion appliance may have a similar problem to some of the Forsus-TAD supported studies in that the endpoint was the desired result (crossbite correction or overjet/canine relationship correction in Forsus/TAD studies) but had differeing amounts of expansion or appliance time. For example, if there is less ‘tipping’ of the molars in the TAD group or flaring of lower incisors in the Forsus/TAD groups then more time or activation is required to achieve the desired result (crossbite correction or overjet correction) and therefore more potential for more skeletal expansion (as in this study) or more skeletal change (in the Forsus/TAD studies – which usually had the TAD supported appliance in longer than the conventional Forsus group). As to the bone width, although statistically significant, a difference in bone width of 0.1 – 0.2mm is questionable as to being clinically significant. As to the nasal cavity changes, it would have been interesting to test the nasal airflow before and after (standardised e.g. using decongestants) and then longer term as IF there is a short term advantage in the nasal cavity change then 1) does it influence nasal resistance (and any SDB if present) short term and 2) does this hold up long term (as well as the expansion). It would also be clinically useful to see patient acceptance reported (discomfort) and any clinical issues/failures during treatment and upon removal. Always easy to sit back and critique after a study is complete but good for future researchers to consider when in the design stages.
Thanks for nice share .
Dr Kevin we are always learning from you.
Well the point is stability and having correcting transverse puts it in the problematic zone and stability might be questionable even with the bone borne RME.
Thanks
This paper is based on Dr. Tugce Celenk-Koca’s Phd Thesis. I personally design mechanism as an clinical instructor and produce the mini implant caps welded to the bone borne appliance. This appliance can be called as an zipper appliance, if necessary you may remove the appliance in every appointment and replace without touching the mini screws. But this feature also has an disadvantage. Clinicians have to weld hyrax screw with at least with 2mm’s pre-opening to insert the appliance. So the appliance lost of the widening capacity of 2 or 2.5mm. When the hyrax screw came to it’s widening limit I offered Dr. Koca to cut one side of the hyrax screw and remove back the hyrax to 2mm opening phase and reweld or after a new impression fabricate a new one. But she prefered to use only one appliance. So to continue to expansion is in the capacity of the bone borne appliance, but in two periods. The limited difference presented in this paper is a result of using only one phase hyrax screw, but not the limited capacity of the fully bone borne appliance design. If you send me your e-mail I’ll forward you the poster that I present the preliminary cases in WIOC meeting Verona 2011. I personally place the screws on these four cases and then Dr. Koca placed all screws by herself with % 100 failure free on all the remaining 16 cases.