Popular posts 3: Be aware of old retainers
One of the most popular posts on this blog was about the potential problems with old retainers. It was unusual to publish a case report. But there was a lot of discussion about this very interesting post,
This is a guest post that is a case report about some problems with old bonded retainers. I thought it was interesting.
This post is by Ken Hansen, Head of the Orthodontic Clinic in Gothenburg. This large clinic employs 17 orthodontists providing care to a population of 500,000. It has an excellent reputation for treatment and research.
Retention
We all know that retention of orthodontic treatment is a dilemma for most orthodontists. For example, Bob Little summarised the findings from the long-term relapse studies from the University of Washington by stating:
“Arch length decreases after orthodontic treatment. Arch width measured across the mandibular canine teeth typically reduces posttreatment, whether or not the case was expanded during treatment. Mandibular anterior crowding during the posttreatment phase is a continuing phenomenon well into the 20-to-40 year’s age bracket and likely beyond”
As a result, many orthodontists practice long-term retention with bonded retainers.
Bonded lingual retainers were first described in the late 1970s. They became more popular during the 1980s and 1990s. Since then, several studies have concluded that bonded twisted retainers effectively keep the anterior teeth aligned. As a result, the multistrand retainer became very popular.
Moreover, due to the depressing findings from Little’s group the tendency to let the bonded retainers stay for many years has increased, at least in Sweden. Orthodontists often delegate retainer reviews to the general practitioner. Unfortunately, some of our patients do not return to their general dentist for regular care. As a result, there is limited long-term monitoring of the retainers. This may lead to problems.
Problems with bonded retainers
There have been a few reports in the literature on the side effects of broken retainers. At the specialist orthodontic clinic in Gothenburg, we have, during the past years, seen some very unpleasant side effects of intact retainers that have been in the mouth for 5- 10 years (Fig 1 and 2). The patients (15-20 cases) were treated in different parts of Sweden so it is not caused by a special brand of twisted wire. It seems as if a twisted retainer wire can start to de-rotate or de-twist after a certain number of years (Fig 3). The progress is probably extremely slow. This means that the tooth may gradually perform a torqueing movement with lingual or buccal root torque.
We should carefully examine all teeth with new gingival recessions that are attached to a twisted retainer. If we see any potential change in root torque, we should remove the bonded retainer and reassess the need for any continuing retention.

Figure 1. A. Patient treated 5 years ago seeking care at the dept. of Periodontology. B. after orthodontic treatment with lingual root torque of 31 and a slight lingual tooth position to put the root back into the alveolar envelope.
 Figure 2. The patient was referred by a general practitioner. The buccal retainer has been in the mouth for more than 10 years. The retainer might be slightly deformed, but the lingual root torque could only be accomplished by de-rotation of the twisted wire.
Figure 2. The patient was referred by a general practitioner. The buccal retainer has been in the mouth for more than 10 years. The retainer might be slightly deformed, but the lingual root torque could only be accomplished by de-rotation of the twisted wire.
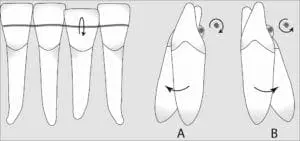 Figure 3. Schematic drawing of a retainer de-twisting, causing buccal (A) or lingual (B) root torque.
Figure 3. Schematic drawing of a retainer de-twisting, causing buccal (A) or lingual (B) root torque.

Emeritus Professor of Orthodontics, University of Manchester, UK.
Hi, I’ve noticed that kind of recession in one of my patients but more frequently, I’ve noticed that they develop tongue thrust leading to unilateral open bites possibly because they start playing with one end of the fixed retainer.
Hi Kevin, do you predict any problems to come with all of the Invisalign retainers that are being put into use? Lots of cases have less than ideal posterior occlusal contact, and we have to let the teeth drift into contact with the trimming of the last aligner trays.
A serious topic indeed! If you want to see more cases, I
co-Authored this report of many similar cases published recently in the AJODO, it was published in the clinical corner section so it’s free access! Here is the link
https://www.ajodo.org/article/S0889-5406(15)01221-4/pdf
Did the patient in figure 1 have any periodontal procedures after the incisor was repositioned ?
Similar findings were reported in this case series by Proffit (PMID: 26827985). The common theme seems to be twisted/braided flexible wires. While these have the advantage of holding the alignment better, wire deformation or unraveling over time can cause some insidious and deleterious effects. Perhaps a stiffer wire (027 SS) bonded only to the canines, but contacting the 2-2 might be a better option. This in conjunction with IPR 2-2 may be a safer long-term alternative (PMID: 25452629)
I have used and taught bonded twistflex splints for nearly 40 years and have found very few problems with them. However, I too have had the odd patient who has experienced the same situation where the wire has caused adverse root torque, after years of follow-up without any unfavourable change. In many of the cases, the adjacent tooth exhibited adverse contra-directional torque. I have also seen the condition occur at an opposing location in both arches, where the teeth involved were the immediate antagonists. These lead me to arbitrarily conclude that the reason was trauma to the wire itself, such as accidental biting on a plum stone, rather than unraveling of the wire.
Prof. Katsaros Bern also have a big collection of this kind of problems. I have the feeling, it’s a clinical and personal feelings, that new solutions like the memotain (lasercut flexible one piece, so not twisted) may be viable solution for long term retention without the fear of de-twisting consequences or strange re-activation due to deformation of the wire. I have personally reduced to 1% breakages of wires in my personal statistics that I am keeping since 3 years, but new studies need to be done on new materials as the digital world opened the space to interesting perspectives.
What kind of twisted wires were used as retainers?
If a rectangular twisted wire is used and some torque is incorporated inadvertently then it may get expressed over a period of time. A passive round twisted wire cannot express torque as per my understanding and experience with bonded retainers for the last 15 years. Possibly distortions got introduced in the retainer wires of the cases shown here that caused labial or lingual movements of the teeth. These cases require deeper examination to find out the correct cause /s of the unwanted tooth movements seen.
Valid points raised Sir. I’d like to add my 2¢:
1) if the retainer wire was a dead soft wire, either flat eg bond-a-braid by G&H (rectangular cross section) or twisted ligature (round cross section), I don’t think it would bring about any kind of torquing effects.
2) if the wire is flexible, either a co axial wire or multistranded rectangular, and it’s countured and adapted and then bonded, it might have over the years resiliency to return to unadapted shape or return to pre manufacturing unbranded shape, which might bring about transverse rotational effects.
3) the force(?) Is it clinically enough to bring about orthodontic movement? Does it even cross the threshold levels of minimum force required?
Regards!
Hi Kevin
I think we’ve all seen this a few times clinically and I’m certain it’s been talked about in ortho forums. Thanks for drawing attention to it. Though I’ve seen it with my own eyes, I am curious about the mechanics of a single point of wire, say a lower central incisor, aberrantly torquing as in the illustrations.
Differential canine torque is unfortunately common as the terminal lengths of the wire untwist. Figure 2 shows this well. However, I’m curious about how if bonding remains intact on each incisor (no wire damage or fraying adjacent to the torqued tooth), how a single point of continuous wire untwists and affects only one tooth? I ask this because I’ve seen this problem on closely inspected intact wires. If the wire untwists evenly the entire incisor segment should show a gentle variation in torque from side to side, not one point.
Perhaps what happens is the incisor’s resin bond lets go so there is no torsional resistance and that one incisor is subject to tongue, lip and occlusal forces by spinning freely on the wire?
Perhaps late lower incisors crowding pressure directed mesially /centrally and the inability of round wires to prevent slipping along the resin pad (like a bracket spins around an 0.018” wire) allows torque to be expressed by squeezing a fan-shaped incisor’s incisal edge buccally or lingually and it becomes crowded out and root torque torque is expressed, just as diagram 3 shows overlapping incisal edges and a torqued root.
Perhaps the wire was not inserted passively at one point? Perhaps the manufacture was uneven in twisting? Perhaps a wire strand was broken and it couldn’t be seen? Maybe the untwisting of a wire at a single site is a simplistic explanation.
I have no doubt that this is a real problem, and I don’t intend to distract from the real problem of the issue, but I don’t see the plausibility of the mechanics of it as noted in the article. The premolar-molar example in Figure-2 makes good sense as it’s the entire length of the wire that untwists, but figure 1 and 3 don’t explain this problem in my mind (which may be the limiting factor here!!)
Ideas, ideas…. Your thoughts?
In any case I’ve heard of annealing the twisted wires before bonding, using braided rectangular wires, etc., as possible solutions to this problem.
Thanks for the interesting post!
The longer you are in practice the more this study seems relevant.I wonder if using rectangular bonded wires would help —it seems to for me –possibly less “unraveling “?
I firmly believe that bonded retainers should be stripped off and replaced every 10 yrs.,at the most,by,definitely ,an orthodontist !
As to how to actually put this into a practical ,practice ,real life situation ?????
The problem I have noticed is not so much the relapse of the previously aligned lower anterior teeth but the excessive amount of wear on the incisal edges with long-term bonded anterior retainers, which I refer to as ‘retrusive bruxism’. I believe IPR would worsen this phenomenon, and stiffer wires might increase the tendency for dehiscence and/or fenestration – it’s a bit like putting handcuffs on for the rest of your life, and restricting the functional behavior of the lower anterior segment.
Hi Kevin, congratulations for your precious blog.
This post remembered me an interesting work by Alessandri Bonetti, Incerti Parenti and Zucchelli titoled “Onychophagia and postorthodontic isolated gingival recession: diagnosis and treatment” published on the Am J Orthod Dentofacial Orthop. 2012.
In the cited article the Authors pointed out the relation between habits such as onycophagia and the abnormal buccolingual inclination of a lower incisor tooth despite the presence of a lingual retainer.
Did the team of Dr. Hansen focused this specific aspect? Do they have an opinion why only some retainers started to “de-twist” in a specific position after a certain number of years?
Thank you.
Matteo
This will happen without a twisted wire. When the tooth crown is squeezed lingually, the root must move labially due to the position of the wire. I noted several cases reported in the AJODO which were improperly diagnosed. Dec 2012 and Jun 2014. My concerns were published in the AJO in Dec 2014
Dr Pickron
We have been aware of this problem for some years. A patients was referred to is some years ago with the root of the lower right canine tooth extruded out of the cortical bone. She had the lower bonded retainer placed a few years previously by a very competent and careful orthodontist. The wire detached on the lower right due to minor trauma and was reattached. The resulting torque twisted the root right out of the bone. Our restorative colleagues found thst the situation was hopeless with severe pocketing all the way to the apex. The tooth was extracted and replaced with an implant.
Since then there have been a number of case reports in the AJODO on this topic and we have stopped using twisflex-type wires for our bonded retainers. We now use a stainless steel chain and teach this to all our trainees
Which stainless steel chain do you use instead? Thank you in advance for sharing.
Hi Niall. Stainless Steel Ortho-FlexTech By Reliance?
I am one of Dr. McGuinness trainees, please allow me to reply to you on his behalf.
Yes, we use the Gold Chain from Ortho-Flex Tech by Reliance.
I have been using Ortho-Flextech from Reliance for many years for my lower 3×3 bonded retainers. Since it is a tightly woven stainless steel chain, the problems in the articles of unwanted tooth movements would be avoided. We all know there is not a perfect retainer but this has served my patients well.
I have encountered similar torquing/ shifting but more often in terminal canines. Sometimes also as narrowing of curvature of upper incisal segment ( presents with small open bite ( not sure if its causative or reactive).
I however, don’t think it is because of inadvertent torque incorporated in wire while bonding as
1. Magnitude of moment/ force applied by dead soft wire should not be enough to torque teeth
2. Even if it is enough it should express within first few month and not after 5-10 years.
3. More likely it appears inability of the dead soft wire to hold tooth position against natural forces, like late mandibular autorotation and or may be trauma of hard food.
I cannot really follow this theory. If the twisted wire should be de-twisted on one side of the tooth, then it must get even more twisted on the other side. The resulting forces and moments are expected to be equal and opposite, so that no resulting moments and movements should be caused.
How about using fiber reinforced composite strips instead of the wires as fixed retainers?
Hello,
it is very important in these cases of “active bonded retainers” to check for external forces caused by nail biting or sucking habits. In quite an amount of cases the phenomenon can be explained by these habits. With nail biting they produce a lingual force on the part of the tooth above the wire what can couse a rotation of the tooth around the wire. I Always combine retention wires with essix retainers to control the 3-dimensional changes. It has to be worn every night 2 years after debonding and after that they have to fit it in once or twice a week to control the situation.
Thank you for this irregular blog. I feel i must share some ideas about long term bonded retainers. To prevent de-twisting, one should heat up both wire ends about 1mm. this allows to adapt it easily to cuspid disto-lingual surface and helps prevent de-twisting.
It is also good to heat-treat the wire, after plying until the wire become gold coloured. Heat treatment restore the alloy to a more stable molecular configuration.
The plying itself must be very careful and should be conducted on a cast.
The wire mus lay just atop the cingulum so the composite can adopt a safe morphology and must look like a bigger convex cingulum without undercuts or concavities. Acomposite brush can help.
Avoid too much rigidity as, when the storm come, the trees can break where the bambou resists.
Kevin
i am disappointed that you have allowed a case based personal opinion to be posted on your excellent EVIDENCE based blog. As the tread shows theses are rare occurrences and there is no evidence based research to demonstrate it is a significant problem. In my own experience, i have had 2 cases where this has occurred in the past 20 years, and i have bonded retainers 90% of all my patients… over 10,000 bonded retainers!
The issue is many orthodontists don’t like bonding over removable, and IMHO that is because we then have to take some responsibly for the bonding process in case it fails, where was a problem with a removable retainer, if it is lost or break we can blame the patient
Bonded retainer have the best retention to enamel IF you minimal prep the surface before bonding (increase bond strength by 60+% (Hadad & Hobson) and if you use a multistrand (eg Wildcat) you get better composite-wire retention (Bearn & McCabe).. using the simple putty jig (Hobson & Easthaugh) with Transbond MIP and flowable restorative composite – it is quick and easy and reliable. Our practice audits show 18% of bonded retainers have problems within 3 mths, drops to 6% by 6mths and 1% by 12 months with failure (meaning a new retainer) 0.8%.
Compared with essix?VFM in the parctices – 30% break /loose/not worn etc within 6 mths (which is better than our local hospital with 77% loss/break/not worn) – so why do we use essix /VFM if the fail rate is double that of bonded?
whenever i ask a group of orthodontists/dentists/nurses/therapsits who have had orthodontic treatment, and 99% have bonded retainers!
However, we still don’t have really good long term (10year+) RCTs to be definitive of one type of retainer over other . Hence IMHO the best is ‘Dual retention’ :- permanently bonded 3-3 + essix worn at nights
Keep pushing for the evidence and drop the personal opinions please
I too have seen the problem. I have been using .0215 braided lingual retainers for the past 30 years and the protrusive incisor root has been a rarity, but nonetheless, an unpleasant outcome for both the patient and for myself. I have reflected upon the cause and my conclusions were much different than those of the author; namely I doubt that a braided wire that is fixed to all the anterior teeth can “untwist” and cause the torquing in the middle of the wire. I see a broken wire almost never and the problem on the lingual only once or twice.
My observation is that the problem is almost always associated with heavy occlusion on the affected teeth as the teeth have settled over time. In this way, the wire becomes the fulcrum and the lingual force on the incisal of the anterior tooth causes the root to move to the facial. Because of this observation, I have become hypercritical of checking the anterior occlusion on retainer checks with tactile sense (fremitus) as well as with articulating paper. Teeth do settle after active orthodontic treatment and if the bite deepens at all, or if late mandibular growth occurs, the result can be the torquing of an individual lower incisor. Occlusal adjustment at retainer checks has seemed to have decreased the incidence to almost never.
When I have noted the problem, I have treated it by leaving the braided wire in place, breaking the composite connection from the affected tooth, and then adding 3 or 4 brackets to the adjacent teeth. With a 17×25 TMA wire (.018 slot), the torque can be resolved within a few months and the lingual wire provides anchorage for the bracketed adjacent teeth. Once the root problem has been resolved, I can rebond the displaced tooth to the lingual wire. Often the gingival problem improves to the point that a periodontist declines to treat it.
Is it possible for twisted round wires to express torque?
Untwisting is just an hypothesis, which is unlikely.. It could be that the lingual wire was not contacting the tooth prior to bonding, so it was forced to contact under tension. This would then create a lingual pull and thus a rotation along the pivot point.
Thanks Kevin for posting this article. Your blog was cited a few times in the last AAO 2018 annual meeting in Washington.
Reading this article and similar articles about Twistflex retainers. Would you say today, having now long term experience and evidence, that Twistflex retainers are contraindicated for further use? (This could have medico-legal consequences). I myself use Bjorn Zachrissons recommended 0.0215 gold plated twistflex wire- although I have suspected seeing this phenomenon ( I then replace the wire, just in case) – I haven’t found a better method of long term retention.
well worth re reading
in my clinics we use a lot of bonded retainers
and we have seen a number “go active” and move teeth adversely
the numbers are very small relative to the number we have placed (500+/year) over the past 10+ years
to draw we have 16 that have gone “active” all are when DBR alone has been relied upon for retention with at least 5years post DBR placement before a problem has arisen
the commonest youth relapsing is a lower canine: with occasional upper canine and the odd incisor
i have retrieved the majority of these retainers and examined them under a microscope and there is no visible “unwinding” of the multi strand wire (we used 0.0175 GAC wildcat which is no longer available) : so that doesn’t explain things
what is in 99% of cases is a failure of bond and it being repaired or there is hisoroty of damage of some form
possibly this may be the cause and more research is required
until we have greater understanding of the limitations of retention i feel dual retention (VFR and DBR) has to be the gold standard
The de-twisting theory can be good in case number 2 – where one tooth moves lingually and the other reciprocally buccally, but according to this theory it is not possible in case of single tooth in the center of the retainer losing torque.
Hi Kevin!
Another emotive topic!
Few points that come to mind when reading your blog and the comments following:
1. We only see what we can see – patients come to me for repair of bonded retainers as their orthodontist has retired, relocated or the patient has relocated. Thus to judge our failures by who walks back into the door may be inaccurate
2. To expect a rigid appliance, of any kind of wire or bonding protocol, placed onto continuously moving teeth (unless ankylosed) and in an ever moving, growing and functional body to last any length of time is perhaps naïve?
3. Taking into account the overall possible risk versus benefit of such a procedure, especially when there are alternatives, I am amazed that there appears to be little related litigation
4. Vacuum-formed retainers of course carry their own baggage, however, the relative risk to the teeth and supporting structure appears less significant (no tooth loss as far as I know), and it is a process that places responsibility back onto the patient, for better or worse. Even in a teen, at some point they need to take responsibility for maintaining their oral health, as they did when they wore their appliances during treatment. There are also possible health benefits for some, such as prevention of attrition and unfavorable loading on weak teeth caused by parafunction at night.
5. I would like to speak to the comment from Dr Savage regarding less than ideal posterior occlusion and Invisalign retainers being trimmed in order to allow teeth to “drift”. If I may suggest a few strategies prior to relying upon “favorable relapse” to finish my occlusion. Firstly the initial occlusion, degree of spacing, retraction, incisor proclination versus retraction required and skeletal pattern may indicate the “risk” of a posterior open bite. As we now know, this is rarely due to the aligner or retainer thickness- , but to transverse or vertical issues preventing full closure ((“incisal interference”, or buccal cusp intrusion (as opposed to palatal cusp hanging with fixed, increasing mandibular plane angle) in the transverse). Next the final occlusion and alignment: using the occlusal contact visualization assists in preventing light or no contact posteriorly, next I would consider the mechanics in place to prevent the 2 main etiologic scenarios – albeit anecdotal – attachment on buccal and buccal root torque in expansion, use of G8 mechanics will assist, (a protocol used by Invisalign to help mitigate or avoid open posterior occlusion), and for me especially watch the incisors during retraction. The inevitable loss of torque – with a fixed or aligner mechanics – may lead to relative extrusion and incisor interference. Finally the staging of teeth – avoiding mesialization posteriorly during anterior retraction, how many teeth moving in the 1 direction during expansion – back to ortho 101 assessing anchorage – this has helped me reduce and avoid less than ideal posterior occlusion, even if not being staged for movement this may occur. “Mind the gap”..
6. Worth a read – Comparative assessment of the survival, stability and occlusal settling between two types of thermoplastic retainers: A prospective clinical trial Bethany Cunning; Alison Sahhar; Sarah Lawrence; David Manton; Paul Schneider Australasian Orthodontic Journal, Vol. 38, No. 1, Jan 2022, 74-87. Speaks to “favorable relapse” and strategies that may be helpful
7. I cant help hoping that we move into the next century with respect to retention protocols. Gluing foreign bodies into mouths – dynamic, never static, “designed” to be functioning and self-cleansing – with unknown / varying ownership or “warranty” period, may have been a logical treatment strategy when majority of patients were teens treated with fixed appliances with little capacity for the steep learning curve required on deband day. In current times with 3D scanning availability, the ability to virtually remove fixed appliances and manufacture removable retainers pre-deband day, the ability to manufacture more than 1 set of removable retainers at an affordable cost, the ability then to store this scan so that minor “relapse” – tooth position change – growth plus relapse – that may occur due to loss may be corrected via manufacturing using the same 3D scan taken pre-deband or at the time of removal of attachments, an increasing number of patients treated with the same geography of appliance as removable retainers so that they are already familiar with the practice of utilization; makes me think that it is time to reconsider our strategies?
8. Please explain to me the logic of placing both a fixed and additionally providing a removable? This practice tells me that we either acknowledge and expect failure of the bonded wire , or that we admit the bonded wire will not maintain the entire dental arch, or that if and when the patient loses or breaks a removable retainer they are not capable of reaching into their cupboard to use the next one that was manufactured at the same time, or that they (or their parents) are not capable of picking up the phone to request the manufacture of a new retainer from the original, completed alignment scan (assuming no significant anatomic change, in which case a 5 minute scan is in order)…
VV speaks for Align Technology