Early Expansion: Patient impacts with RME versus quad helix.
The open-ended discussion around expansion in orthodontics is ongoing. While not everyone is convinced of the merits of early expansion, the conversation has moved on and now encompasses the use of much more invasive surgical means of correction. Nevertheless, non-surgical approaches to achieve dental or skeletal expansion remain in vogue, with the quad helix (QH) and rapid maxillary expansion (RME) remaining in routine use.
Both appliances will likely produce some negative patient impacts, being bulky and occasionally cumbersome. I’m not too fond of the quad helix, in particular. I tend to feel that it is an appliance producing dental change only, often leading to somewhat uncontrolled expansion, may require multiple phases, and often induces transient unwanted side effects. Therefore, I tend to feel that there are more sophisticated alternatives which will lead to dental expansion and allow simultaneous correction of other issues. On the other hand, RME will predictably induce both skeletal and dental changes. The latter, therefore, may have a telling effect on space conditions and, ultimately, treatment outcomes.
In this study, the authors evaluated the patient impacts of early expansion with a quad helix versus RME
A team from Sweden did this study.
Stina Hansson, Eva Josefsson, Rune Lindsten, Anders Magnuson and Farhan Bazargani
What did they do?
They conducted a two-group randomised controlled trial involving 72 participants as follows:
Participants:
Participants had a unilateral posterior crossbite and were in the early mixed dentition with maxillary first permanent molars erupted and the primary maxillary canines and second primary molars retained. Molar relationships were Class I or II with a maximum overjet of 5mm.
Intervention Groups:
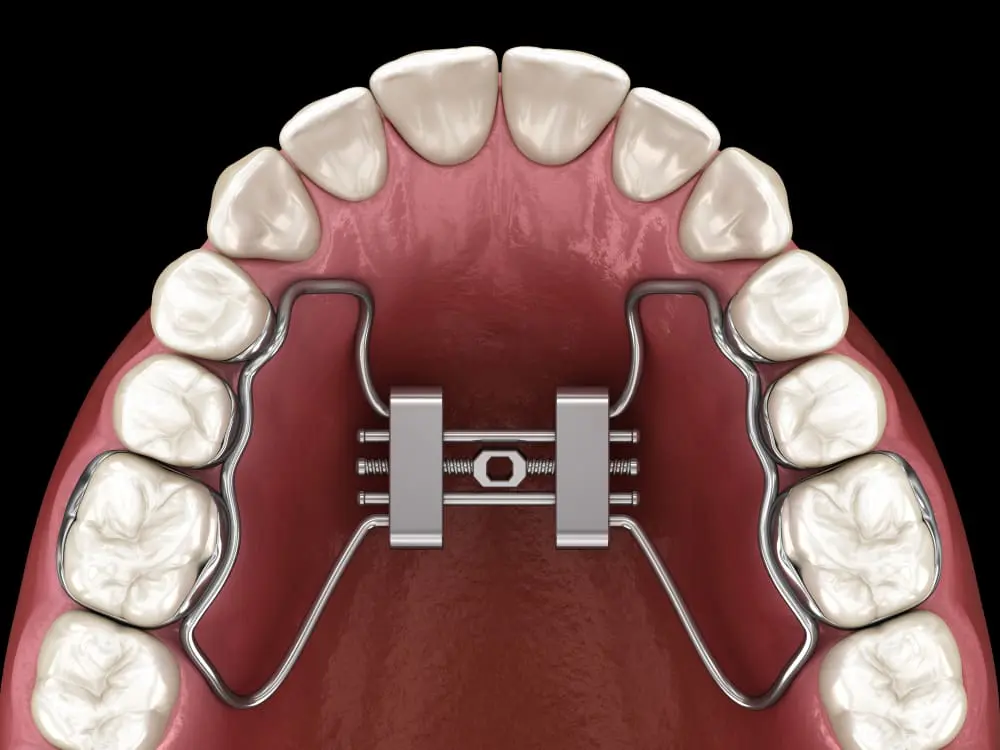
The QH involved a 0.9mm stainless-steel wire with bands on the first permanent molar. The operator used a Hyrax RME device with a 13-mm expander. It was cemented to bands on the second primary molars and bonded to the primary canines with a rest seat on the primary canine using a flowable composite. They cemented all bands using glass ionomer. Posterior bite blocks were added to the second primary molars in both groups. The RME was activated by 0.2mm twice daily until the palatal cusp of the upper first molar approached the buccal cusp of the mandibular first molar. The QH was activated by one molar width before cementing with reviews at 6- 12-week intervals until normal transverse relationships were achieved. Experienced clinicians in two centres performed all the treatments.
The participants completed questionnaires exploring pain intensity, discomfort, analgesic consumption, and functional impairment on treatment’s first, fourth, and seventh days.
What did they find?
The team collected data from almost all participants (35 per group), with the groups perfectly matched in terms of both age (9.5 years) and gender (37% female). Forty percent reported discomfort during the insertion of the appliances, with no difference between the groups. The pain was greatest on day one, subsiding by day 7. The QH group experienced more pain from the tongue and more chafing from the appliance up to day 4. By day 7, no significant differences were observed between the groups as the pain had declined.
Analgesic use was common on day 1 (QH: 46% and RME: 35%), reducing to 14% in both groups by day 4, with none needed after seven days. Six children (approx. 1 in 6) in each group took the first day off school due to pain (I am not sure I would be this lenient to my children!). They saw slightly more speech impairment with RME on days 4 and 7.
What did I think?
This was a helpful study. There has been a lot of talk about including patient impacts and experiences in research studies. While this may be happening more, I think this data often gets lost amid objective clinician-focused data. I am sure this paper will be coupled with a separate report detailing the objective effects of appliance therapy. I am also almost certain this will show near-uniform objective treatment success with more skeletal effects in the RME group. Therefore, we must give sufficient emphasis to the patient-centred data. Equally, we are all increasingly attuned to the need for more clinical trials (and arguably less secondary and tertiary research). A dedicated paper detailing patient-reported data from this clinical trial is, therefore, I think, the best approach.
The methodology and writing are clear, and the authors have written the paper nicely. It would therefore be easy to replicate this study or perform a similar study evaluating the potential merit of other modifications or designs, particularly given the flexibility offered by contemporary approaches, including CAD-CAM designs.
The pattern of pain experience and patient reports closely mirrored those observed with standard multi-bracket fixed appliances. Specifically, the pain seemed to peak by 24 hours before virtually being eliminated at seven days. It does appear, however, that more discomfort arose with the quad helix than with the RME. As per my earlier comment, I probably have a personal bias against the quad helix, but should this information be another reason to be even more selective around their use?
A limitation (but arguably also a strength) of the study was the focus on patient experiences. Objective data around short- and longer-term treatment outcomes would also be interesting. In particular, longer-term findings considering the relative stability of the change produced with both appliances will be of value and interest.
What can we conclude?
Young patients (aged 9 to 10) tolerate both RME and QH. The pain experience is similar in severity and course to that arising with multi-bracket appliances. However, irritation of the tongue is common, particularly with the QH. This information should help us in setting expectations for our pre-adolescents, who we feel might benefit from early expansion.

Professor of Orthodontics, Trinity College Dublin, The University of Dublin, Ireland
Thank you for sharing this study and your thoughts on this matter.
It would have been good to have included in this study one important consideration.
What is the parent experience and which appliance is less stressful?
I’ve always believed that the parent having to turn the RPE made this appliance less attractive in regard to the entire experience.
The discomfort issues with the quadhelix can be lessened with planning and/or proper adjustments at delivery.
The RPE has more issues with loosening or the parents inability to make the necessary activations.
It has been my experience that the RPE issues seem to more often result in extending over all treatment and chair time.
As was the case for this review Padhraig, unfortunately, most published trials regarding RME intervention for children who are afflicted with Dx:Maxillary Transverse Skeletal Deficiency (MTSD), still continue to list as primary inclusion criteria (at T-0) the presence of a posterior dental cross-bite, and also, the stage of dental development to be during the early/middle/late mixed-dentition; that is, the subjects are NOT still in their full deciduous dentitions (under 72 months of age) when MTSD is most often first detectable, known to reliably persist beyond and will often already be, or will later become, a co-morbidity with sleep and respiratory hygiene problems, impaired QOL and also sometimes conductive hearing loss, bedwetting and compromised general health (myriad references upon request dating from 2023 back to the early 20th-Century). Many of our our colleagues are now identifying kids at risk (with scientifically-validated screening/risk assessment tools such as the Pediatric Sleep Questionnaire, etc.) for Early Childhood (skeletal) Malocclusion (ECM-under 72 months of age) with/without Sleep Related Breathing Disorder (SRDB), etc. co-morbidities. Should you Padhraig, and hopefully some of your readership, be interested in exploring this concept further, please check out what is scheduled for later this month at the American Dental Association’s headquarters in Chicago (https://www.ada.org/en/education/continuing-education/ada-ce-live/childrens-airway); it is only live/in-person attendance now but plans to record the 3-day event will allow for later viewing.