Using skeletal anchorage for expansion is not necessary in pre-adolescents! A five year follow up of a trial.
Expansion appears to be all the rage at the moment. There are claims and counterclaims for its effects and benefits. Indeed, the discussion is getting very heated. Strangely, most of the claims are based on selective quoting of convenience studies with low levels of evidence. I have discussed expansion many times on this blog, and it has been challenging to come to solid conclusions. We also have to consider the type of expansion we should use with respect to skeletal anchorage. This was summarised nicely by Martyn Cobourne in a recent post on this blog. He concluded
“Bone-borne expansion seems to be the future. First, however, there is a need for some high-quality clinical trials to investigate further and refine these appliances”.
This new study sheds some light on this subject. It was also unique as the authors report data five years following expansion.
A multinational team from Sweden, Germany and Russia did this study. The European Journal of Orthodontics published the paper.
Bazargani et al. EJO: Advanced access. DOI: https://doi.org/10.1093/ejo/cjad024
What did they ask?
They did the study to:
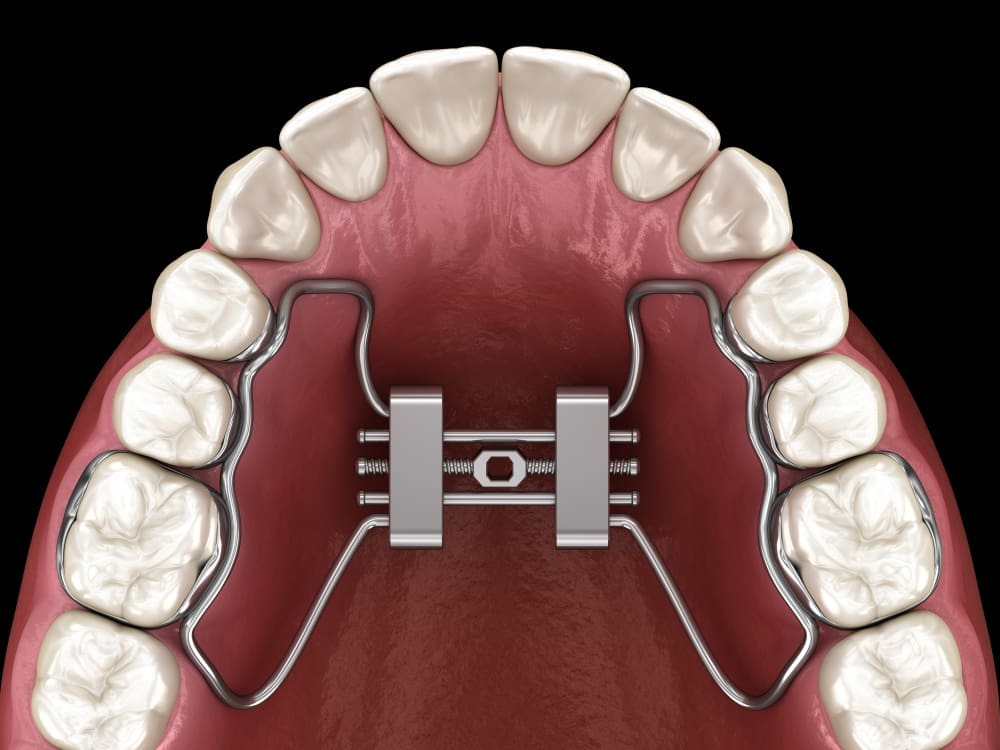
“Three dimensionally assess and compare the influence of the conventional Tooth Borne-RME and Tooth-Bone-Borne RME (skeletal anchorage) on the skeletal structure of growing children”.
What did they do?
The team did a single centre two-arm parallel-sided RCT. This study started enrolment in September 2010 and closed in December 2015. The PICO was:
Participants
Patients aged 8-13 with unilateral or bilateral crossbites with constricted maxilla. Their dental age was in the early or late mixed dentition.
Intervention
Tooth borne RME (TB).
Comparator
Tooth-bone- borne (TBB) RME with skeletal anchorage
Outcomes
Primary outcome: Mid-palatal suture expansion. The secondary outcomes were skeletal expansion at the nasal base. The marginal bone level at the buccal aspect of the first molars and any skeletal differences between boys and girls.
The team collected data at the start of the study, at the end of the expansion, one-year post-expansion and five years post-expansion.
The primary data sources were CBCT examinations at all the data collection stages. They derived most of the measurements from the scans. Their statistics were relevant.
Importantly, the authors used a pre-determined randomisation that remotely allocated the interventions. Notably, the allocation was done after the patients entered the study. A research assistant revealed the allocation to the operators, ensuring good concealment. They analysed the data blindly and did a nice sample size calculation based on the differences in palatal expansion between the two techniques.
What did they find?
They enrolled 52 participants in the study and they all completed treatment. One participant in each group missed their CBCT appointment at the end of the expansion. They analysed data on all the participants after five years.
Similarly to most orthodontic studies, the authors presented a ton of data. I have decided to concentrate on the primary outcome of palatal suture expansion and nasal width.
In short, they showed that at the end of expansion (T1), the mid-palatal width difference was 0.6mm (CI 0.2-1.1) greater in the TBB group. However, this was not evident at the last data collection points.
When they looked at nasal width at T1, it was 0.7mm (CI 0.1-1.4) greater in the TBB group. At T2, it was 1.6mm (CI 1.0 -2.3); at T3, it was 2.1mm (CI 1.4 -2.8).
All other outcomes showed either no significant differences or were clinically insignificant.
The authors concluded:
“Skeletal expansion in the mid palatal suture was higher in the TBB group. However, this may not be clinically significant”.
“Skeletal expansion at the level of the nasal cavity was higher in the TBB group”.
“The use of miniscrews and skeletal anchorage in young preadolescents cannot be recommended due to the similar outcomes as the less invasive conventional TB-RME”.
What did I think?
This was an excellent study that used high-level methods. I was also impressed that the study team successfully followed up participants for five years. In many ways, this makes this study unique. Their methodology was sound, and the paper was very clear.
When I started to read the paper, I was concerned about the repeat CBCTs. I have been critical of other retrospective studies using multiple CBCTs. However, in this study, the team got ethical committee approval for the CBCTs, and this deals with ethical issues, as the patients would have been fully informed.
The authors drew attention to a systematic review that showed mini-screw assisted RME produces more significant expansion than tooth-borne expansion in late adolescents. This led them to conclude that there is no need for mini-screw expansion in the mixed dentition. Effective treatment can be done with a tooth-borne RME.
Interestingly, it flies in the face of most of the stuff currently peddled by the airway/expansion groups. It would be great if they read and understood this study.

Emeritus Professor of Orthodontics, University of Manchester, UK.
Over a 43 year career, I’ve done lots of expanders both tooth borne and bone borne. I really enjoyed this paper. My only question would be does the tooth borne expander work better if there are more than two anchor teeth? And by that I mean, more than two anchor teeth included in the appliance in a fixed way, more than just a wire touching the lingual surface.
This is an excellent study.
Part two of this study should be an analysis of the difference between residual facial alveolar bone, 5 years post treatment.
Colin Richman DMD.
I am also of mixed feeling about the repeat CBCT exposure the sa
Miles or patients had to undergo. If the onlly objective was to identify expansion that had occured 3D scan was just right enough. What is the role in evaluating the expansion of nasal floor width is another question that comes to mind. Was it a therapeutic goal during the treatment ?
I have not read the paper, but would like to understand why the nasal width continued to increase at a greater rate in the bone borne expansion group compared to the non-bone borne expansion group over the 5 year observation period? What is the basis for this and did the researchers compare other relevant factors such as airways function and facial growth pattern between the two groups?
As a student, I was taught to read the entire radiograph. Using that a priori approach, I found an anomaly in Figure 3 of the paper. It appears to show rhino-ethmoidal sinusitis. The question that arises from that observation is: Does expansion have any therapeutic role in sinusitis? In one study (Ref below), increasing the nasal width thru non-surgical expansion appeared to resolve maxillary sinusitis. Using the same empirical approach, the second question that came to mind was: Are there any post-maxillary changes? The reason why this is relevant is because various forms of surgical expansion (MARPE, SARME and DOME) are associated with iatrogenic pterygopalatine fracture, but it was not possible to discern that from the data provided in this study.
Singh GD. Sino-nasal changes associated with midfacial expansion: An overview. In: Paranasal sinuses anatomy and conditions. InTechOpen 2022. ISBN 978-1-83969-690-9.
Dr. Wong published some of his results a couple months ago during a lecture, they were doing tooth-borne expansion in kids around this age. They were really impressed, I commend them for showing the CBCTs but all I saw was dental tipping. Pushing teeth in order to affect the bones of the face seems like a horrible idea if you ask me, whether it’s a 30 year old, 20 year old, or 10 year old.
I’m having a really hard time differentiating between expanders that utilize an RPE element (even MARPE + RPE hybrids) and DNA/ALF appliances. The CBCTs look almost identical to me.
Maybe you get a little tiny diastema and opening anteriorly with the MARPE.. Not good for breathing, not good for the face, all it’s going to do is give you a wide nose and big mouth.
I think the MSE cases by Won Moon were better but there was lots of failures in >20 so people put the appliance as anteriorly as possible and put arms on all the teeth.
3 CBCTs on patients 8-13 for 2 exposures and I assume 13-18 for the 3rd CBCT.
I suppose that says says something about the ethics committees and the peer review process for the EOJ. Were any of the 3 exposures necessary and usual for treating that individual? Fairly obviously the 2nd and 3rd exposures were only risk and not benefit to the individual patient.
I am very surprised this paper was published and it raises ethical questions when we reference it, it gives praise to authors for unnecessarily exposing their patients to ionising radiation (that may harm and is not to that individual’s benefit).
‘First, do no harm.’
I would advocate for the withdrawal of the paper.
Thank you for reading our article. I understand and share your concerns about CBCT usage. In my practice, I personally use the CBCT machine only 1 or 2 times a month.
Our project, initiated by Farhan Bazargani in 2009, was inspired by Cervidanes and Hugo De Clerk’s groundbreaking work on bone-borne appliances using Björk’s structural superimposition technique. This led us to investigate the superiority of bone-borne expanders (hybrid-HYRAX) compared to tooth-borne expanders.
Initially, I believed that bone-borne rapid maxillary expansion (RME) would outperform other methods. However, over a five-year period, the superior effects diminished, which was both frustrating and understandable. It’s important to note that our results focus on the long-term effects after five years in a specific age group using the hybrid HYRAX appliance.
To address the need for clarity on the benefits and drawbacks of this procedure, we specifically targeted a vulnerable group of young patients.
Based on our study’s long-term outcomes, we found that bone-borne expanders (hybrid HYRAX) do not outperform tooth-borne alternatives within this specific age group. The use of bone-borne expanders in young children is limited and may be appropriate for cases of agenesis or certain class III cases requiring maxillary protraction without adverse effects on dentition.
Regarding ethics, the committee had no concerns about CBCT scans, and we have an approved protocol in Swedish. We strictly adhered to the ALARA principle when adjusting the CBCT scan dosage, which aims to minimize radiation exposure while ensuring diagnostic image quality. In comparison, classical x-ray diagnostics using digital panoramic and lateral cephalometric radiographs resulted in effective doses of 21.5 and 4.5 μSv, respectively (Am J Orthod Dentofacial Orthop. 2012 Apr;141(4):436-43. doi: 10.1016/j.ajodo.2011.10.024). Close collaboration with the radiological team in a hospital or university setting allows for proper dosage adaptation.
One advantage of our study’s 3D accuracy and volume superposition technique is overcoming challenges associated with 2D imaging, such as inaccuracies and overlapping anatomical landmarks.
Dear Bjorn, thank you for your reply.
I understand the desire for improved knowledge and the comparison you used. I liked the way the stats were presented (much) better than usual with confidence intervals and effect sizes. There are many pleasing facets to the article. The results are important, they affect our decision making, however, I have very mixed feelings in using them. But …. I cannot work my way around the repeat and 3peat CBCTs which were not diagnostic and not for the individual patients’ benefit.
Even with a signed informed consent stating that 2 later CBCTs would be obtained that would not benefit the individual and would lead to (a small) increased risk of brain, thyroid and eye tumors later in life I find it difficult to comprehend how this study was allowed. The European protocols for research on humans reads as if they are very strict.
I would prefer a world where a patient experiences no risk as we seek better answers to our questions. Perhaps the cost of answers and knowledge is too high and we need to better accept uncertainty even as we strive for improved methods. Not surprisingly, I personally would not have done this study, I suspect others would have found too many obstacles to allow them to proceed as well.
Thank you for your professional response, which I fully understand and appreciate. I don’t intend to defend anything because your perspective is relevant. The European regulations regarding radiation usage are extremely strict, and the ethical committee in Sweden carefully evaluated this situation. As mentioned earlier, significant efforts were made to adapt the dosage accordingly. If you’re interested, the lead researcher is willing to share the ethical approval and protocol to provide you with a better understanding. Please send a private message if you’re interested in this information. Once again, I want to emphasize that this is not meant to be a defense or disagreement with your statement, as I would likely express a similar viewpoint from your perspective. You can reach me at [email protected]. Thank you for the professional and important discussion.
Use of CBCT, solely for the purpose of data collection, with no therapeutic benefit to the patient, in a actively growing stage- definitely harmful, as of current standards. The ethical committee approval as well as the peer reviewers’ recommendation for accepting the paper for publication is highly suspicious, to say the least. This might also open floodgates of n rampant ‘growth/clinical studies’- with multiple CBCT exposures of dubjects during growth spurts!