Is orthodontic root resorption a problem? A new systematic review
Orthodontic root resorption is a common “side effect’ of orthodontic treatment. This systematic review gives us new information on this problem.
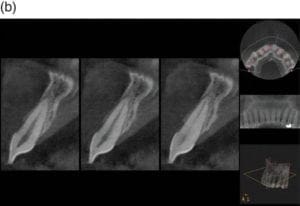
We are all familiar with Orthodontically Induced Root Resorption (OIRR. Several studies have related the amount of resorption to many possible causes, for example, the duration of treatment, appliance type and forces applied. While these have provided us with useful information, most have used 2D radiographs. Recently, CBCT imaging has allowed more accurate measurement of OIRR. As a result. the authors did this new study to answer this question:
“What is the mean amount of OIRR measured with CBCT imaging”?
A team from Thessaloniki, Greece did this study. The EJO published the paper.
A Samandara et al
EJO on line: DOI:10.1093/ejo/cjy027
What did they do?
They did a standard systematic review of the literature. The PICO was;
Participants: Orthodontic patients in the permanent dentition.
Intervention: Orthodontic treatment
Outcome: The amount of root resorption measured by CBCT imaging.
They used well established systematic review methodology and carried out electronic database searches, precise data collection and assessment of risk of bias of the studies. They included RCTs and retrospective non-randomised studies. I will expand on this later.
What did they find?
They identified 30 publications. Six of these were RCTs, 6 were prospective non-randomised studies and 18 were retrospective studies. These included data on 1219 patients whose age ranged from 11-4-26.6 years.
They felt that 4 of the trials were at high risk of bias. Importantly, all the non-randomised studies were at high risk of bias.
They presented a large amount of data in the text and in detailed tables. I have condensed what I felt were the main findings into this table.
| Mean OIRR and 95% CI (mm) | |
| Fixed appliance | 0.8 (0.5-1.0) |
| RME | 0.4 (-1-0.7) |
| Anterior teeth | 0.9 (0.6-1.1) |
| Posterior teeth | 0.2 (-0.3,-0.8) |
What did I think?
I thought that this review could have provided us with important information and I am sorry that I being “lukewarm” about their findings. However, we need to be careful when we interpret the results. This is because they included retrospective studies in the review. Importantly, they classified all these studies as being of high risk of bias. Unfortunately, this simply results in a review that is biased. It is important for us to consider that if a systematic review is going to be of value, then it should only include RCTs.
Nevertheless, they carried out a sensitivity analysis that showed that the retrospective studies tended to show greater OIRR (1.0mm) than the prospective studies (0.6mm).
In summary, I feel that we can conclude, with some caution, that when CBCT is used to measure OIRR, the average amount of resorption is 0.6-0.8mm. This is a small amount and is reassuring.

Emeritus Professor of Orthodontics, University of Manchester, UK.
 Evaluation of orthodontically induced external root resorption following orthodontic treatment using cone beam computed tomography (CBCT): a systematic review and meta-analysis.
Evaluation of orthodontically induced external root resorption following orthodontic treatment using cone beam computed tomography (CBCT): a systematic review and meta-analysis.
I don’t think orthodontists are too concerned about the average amount of root resorption if it is in the .6mm range. I am more concerned about the end of the bell curve and the risk of more extreme root resorption (3mm or more). What is the overall risk of those events and what causes it? Just empirically, based on my years of providing orthognathic surgery care to a post adolescent/post orthodontic tx military population, the biggest risk is iatrogenic in nature. The worst resorption seems to be seen in skeletal open bites treated with long term vertical elastics. A subset that seems particularly susceptible is the progressive open bite case due to condylar resorption. Treat this case with vertical elastics and the root resorption can be quite catastrophic.
This is an interesting observation – Do you mean the molars or the incisors are more susceptible to the resorption?
Does it matter that there is no mention of a control here? I presume we can expect no resorption in the untreated patient but has anyone demonstrated that?
Also – for some younger patients, are all roots fully formed when they take the initial measurements? I imagine a lot of ortho begins before premolar and upper canine apices are closed, so how do we know what they would have grown to?