CBCT imaging does not meaningfully change decisions on impacted canines?
We all know that CBCT gives us great images of impacted teeth. We can justify this additional radiation dose if the images improve our decisions. However, there is little evidence on whether this is the case. I have posted about this before, and there was a very active discussion on my posts. Several years have passed, and I was interested in this new paper. I wanted to see how the situation has changed (or not).
One of the most logical reasons to take a CBCT image is when we are managing impacted teeth, particularly when there is suspicion of root resorption. However, few “real-world” studies have assessed the value of taking additional CBCT images and exposing a child to an increased radiation dose. This was the focus of this new study.
Peter Stoustrop et al
EJO: Advanced access. DOI: https://doi.org/10.1093/ejo/cjad062
A team from Aarhus, Denmark did this study. The EJO published the paper.
What did they ask?
They asked:
“What is the impact of cone beam computed tomography on treatment planning for impacted maxillary canines”?
They were also interested in gathering details about the variables that might have contributed to a modification in the treatment strategy and identifying any indicators suggesting the need for an additional CBCT scan.
What did they do?
The team conducted a prospective clinical observational study on the treatment decisions made by 10 orthodontic specialists.
The study had several stages.
- The team identified patients with at least one impacted maxillary canine, and the initial 2D radiographs showed an overlap between the canine and adjacent teeth. In other words, the orthodontists were concerned about root resorption.
- A referring specialist orthodontist initially saw the patient and took 2D radiographs. The orthodontists then referred the patients to Aarhus for the CBCT.
- Before the orthodontist referred the patients, they recorded relevant clinical factors about the canine. These included, for example, whether there was adjacent tooth resorption and the position of the canine. They also prepared their treatment plan based on the 2D imaging.
- A radiologist then reported the CBCT images. The referring orthodontist then viewed the report and the CBCT. The orthodontist then formulated the the final treatment plan.
- They then used the relevant logistic regression analyses to compare the treatment plans and decision changes.
What did they find?
They included 125 impacted canines from 91 patients in the study. These were referred by 10 specialists with experience ranging from 1 to 28 years.
When the new treatment plans were devised. They found a modification in the plan for 34.4% of the canines. The most common alteration involved a change in the direction of orthodontic traction. This was subsequently followed by the extraction of other teeth (12.8%) and the surgical exposure of the canines (10.4%). Notably, in only 3 cases was the plan adjusted from extraction to retention of the canines.
When they examined root resorption, they discovered that 67 teeth were diagnosed with resorption following CBCT, whereas with 2D imaging, this was only 9. However, the analysis did not reveal any impact of CBCT-diagnosed root resorption on the treatment plan.
Finally, when they looked at factors from the 2D images that could identify the best patients for additional CBCT imaging, they found that a significantly larger alpha angle was associated with changes in plans towards removing the canine.
Their most important conclusion was;
“The CBCT images resulted in a change in the treatment plan for approximately one-third of the canines. This was mostly a change in the direction of orthodontic traction. The least frequent change in plan was the decision to remove the canine for only 4 cases.”
Importantly, although the CBCT images provided much additional information, their use did not significantly impact the treatment decisions.
What did I think?
This was a well-done study that looked at a clinically relevant question. Unlike other studies in which orthodontists examined specially prepared case records, this study looked at patients in a “real-world” setting. Importantly, the orthodontists examined the records from their own cases. This adds externality to the study.
We must also remember that these cases were selected because the orthodontists suspected that adjacent teeth were resorbed. The CBCT views were also targeted on the patient’s initial examination. Importantly, these were not CBCT images that had been taken as part of a “routine” set of records.
As a result, the finding that there was only minimal change in the decisions is even more important. This is because if these changes are minimal in targeted patients, it is very unlikely that “routine” CBCT imaging would add any further relevant information. I accept that my view may be controversial. However, we cannot justify exposing young people to increased levels of radiation “in case we find something”.

Emeritus Professor of Orthodontics, University of Manchester, UK.
A CBCT scan could be more helpfull for the surgeon than the orthodontist. We should ask the person who performes the exposure..
I agree that the CBCT doesn’t often alter the orthodontic plan per se, but in my experience (irrespective of whether the CBCT is taken by the orthodontist or surgeon) it can fundamentally change the surgical plan. The starkest example of this occurs when the surgery no longer requires a full exploratory palatal flap to be raised (requiring a GA in most UK clinical settings) because a much more targeted exposure with a small or no palatal flap is feasible (for an open exposure). This change has occurred because the surgeon is much better informed about the 3D location / orientation of the canine and adjacent roots, plus bone coverage, as a result of CBCT imaging.
From a patient (or parent’s) perspective this makes a crucial difference in the clinical management since the surgery can be performed under LA not GA. This, in turn, reduces costs, delays in surgical exposure and morbidity.
Therefore, perhaps the question about CBCT and ectopic canines should be how often it alters surgical management and not the orthodontic treatment planning.
There is a tendency to generally associate a CBCT with a high radiation exposure. However, with the ultra low dose modalities of modern devices, a CBCT of the entire upper jaw can be recorded with half or a third of the radiation dose of an OPG. Therefore, the question should not be if one should use a CBCT or not, but one should ask oneself whether the “invested” radiation dose is worthwhile for the information obtained.
Dear Sir,
Thank you for this post and reminding us that care is an essential part of Orthodontics.
It is sad and terrible if there are still places where CBCT is done as part of “routine exam”. After decades of common knowledge that a new patient Pantomograph is just criminal negligence (even though the law may be lax in this regard), a higher radiation-dose CBCT is only of value if we are trying to determine which tooth to save in case of 50/50 suspected resorption. I agree with the previous comment that one way of reducing the need for CBCT even further would be to let the oral surgeon decide during surgical exposure and bonding of the impacted canine whether they need a 3-D view. Once the flap is raised, the surgeon can see more detail than any CBCT image can provide.
Every healthcare discipline proceeds with caution when irradiating children, Orthodontics is and should be no exception.
Thank you.
Yours sincerely,
Mr Karun Sagar, BDS
Orthodontic Assistant
This is my ignorance
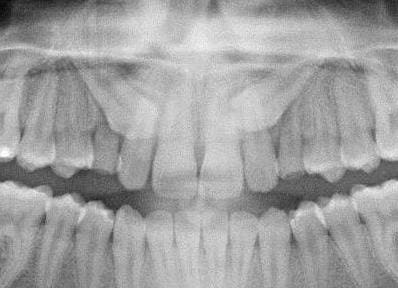
When the canine crown is occlusal to the lateral apex (such as the upper right canine in the introductory jpg
https://p.feedblitz.com/t3/977344/71077093/14285666_/~kevinobrienorthoblog.com/cbct-does-not-meaningfully-change-decisions-on-impacted-canines/?utm_source=rss&utm_medium=rss&utm_campaign=cbct-does-not-meaningfully-change-decisions-on-impacted-canines)
does resorption of the lateral root at the lateral apex occur? Or has anyone seen resorption bisect the lateral, leaving apical lateral remnants?
Can a CBCT indicate false positives? That is can the resolution of a CBCT read as resorption when there is none?
(The reason for this question is a CBCT indicating root dehiscence is frequently accompanied by intraorally exhibiting no soft tissue dehiscence implying the possibility of periosteum and thin bone below the CBCT resolution, or at least that’s my interpretation because I’ll be darn if I’m going to lay a flap or probe aggressively and create the soft tissue dehiscence.)
Thanks
Again a question revealing perhaps my ignorance
Does marsupialization of an ectopic canine follicle eliminate the potential for resorption? That is, does extraction of the primary canine (perhaps a focal marsupialization) or an open exposure of the ectopic canine, eliminate the potential for resorption or continued resorption and mitigate the need for a Phase I whose purported purpose would be the concern for resorption?
Thanks
In the discussion , there has been no mention of the line of action if the force that needs to be applied to move the canine safely away from the incisor roots. I am aware of several cases where the clinician has been unsuccessful in erupting the canine . Then a CBCT was taken which demonstrated that the line of action of force was incorrect. The line of action of force was then correctly adjusted and applied and the canine erupted. In some situations a moment has to be applied where the canine root is hitting the first premolar root. 2D imaging does not allow clear planning of the line of action of the force. In these situations, the clinician will increase his risk of liability / litigation even if proper consent is obtained. Furthermore , an incorrect line of action of force could also cause iatrogenic root resorption of the incisor roots. Not to mention the increase in treatment time and the associated problems longer treatment times will cause. Lastly, there is the question of the clinician and the level of his experience in bringing down impacted canines. Guidelines is one factor, but if the clinician feels that he would benefit from having CBCT information, then why shouldn’t he take this image until they have enough experience over time to decide where they can safely take the chance of better selecting cases where a CBCT is necessary or not. In the UK , we also have a system where a clinician is forced to treat impacted canine cases in many areas of the country and cannot necessarily refer some patients into the hospital for treatment.
I take a limited field of view conebeam of impacted teeth to determine if they can be exposed in my office with a laser. I rarely have to refer to an oral surgeon anymore. Also, determining the direction of force is important. If you pull the canine into the roots of another tooth you are going to resorb the root or the tooth won’t move.