Breathe..breathe in the air: a classic paper on breathing and facial growth.
Breathe..breathe in the air: a classic paper on breathing and facial growth.
Since I started this blog I have become aware of orthodontists and dentists who work in the area of breathing and orthodontic treatment. So I thought that I would post on one of the classic research papers in this area. This is a controversial area but it is not new and many of the clinicians who promote breathing related orthodontic treatment (BROT) quote this paper.
Mandibular growth direction following adenoidectomy.
Linder-Aronson, S., Woodside, D. G., & Lundström, A. (1986).
American Journal of Orthodontics. doi:10.1016/0002-9416(86)90049-7
Several real ‘giants of orthodontics’ wrote this paper, and there is no doubt that their influence on our specialty is immeasurable. This is one of our classic papers and is required reading on most specialty programs.
I have decided to review this paper using our knowledge of current research methods. Nevertheless, we need to remember that this paper was published in 1986. This was a long time ago. I had just completed specialist training in orthodontics and Manchester United were a mid-table football team. In those times, clinical orthodontic research was in its infancy, studies were dominated by cephalometric measurements and statistical and research methods were rather simple. So please, do not think that I am being overcritical about this study. I am sure that if my publications are reviewed in 30 years time, the reviewers would be very critical. Bearing this in mind here is my analysis of this paper.
What did they ask?
The literature review was extensive and they pointed out that there was increasing evidence from animal experiments that vertical growth was a consequence of the chronic impact of environmental influences. They expanded the review to describe the many environmental factors that may influence facial growth. Most of this evidence came from observational studies on humans or animal experiments.
The aim of their study was to determine whether the establishment of normal breathing in children with severe nasal obstruction affected mandibular growth direction. The null hypothesis was
” the establishment of nasal respiration in children with severe nasopharyngeal obstruction will not affect mandibular growth direction”.
What did they do?
They selected a group of 81 Swedish children who had undergone adenoidectomies to relieve severely obstructed nasopharyngeal airways.
48 of these children changed from mouth to nose breathing and this group formed their initial sample. They then followed 38 of these children for five years. This was their final sample.
All the children had the following records collected;
- Study models
- Lateral cephalometric and PA radiographs
- Airflow measurements recorded by rhinometry
At the following stages;
- T0 Before operation
- T1 1 year post-op
- T3 5 years post-op
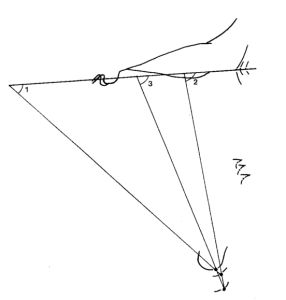
Donald Woodside traced the radiographs and superimposed the tracingson the anterior cranial base. He then measured the change in position of gnathion relative to Sella-Nasion. As shown in this diagram.
They carried out a very detailed error analysis and this showed that the method error was 8° (but I found this very confusing).
They analysed the data with univariate statistics. Importantly, they analysed the data from the boys and the girls separately and I could not find the rationale for this step.
What did they find?
They provided a lot of data in the forms of graphs and table. In summary they found the following:
- Girls who had adenoidectomies had more horizontal growth than the girls in the control group. The difference in the position of gnathion was 11.5 degrees and the 95% Ci was 2.25-20.75 (which is very wide)
- This difference was not found for the boys
- Growth direction was more variable for the adenoidectomy group than the control group
- The mean airflow through the nose increased for the adenoidectomy group
In their discussion they pointed out that their sample was biased because it only included those children who changed their mode of breathing. There was then a further sample attrition of 10 more children.
They pointed out that they could have carried out a trial that this was not possible for ethical reasons.
The final conclusion was that there was an association between adenoidectomy, with a change mode of breathing, and the establishment of horizontal growth for girls.
What did I think?
There is no doubt that for its time this was a classic paper and it is important to point out that the authors acknowledged that there were biases in a sample. These were associated with the following:
- The study was not a trial and there was no untreated control group
- They only analysed the patients who became nose breathers, they excluded those who did not respond to the treatment.
- They did not present data on any differences between the treatment and control groups.
- There was considerable attrition in the study
- The mean error of measurement was large, bearing in mind the small differences that were detected by the cephalometric analysis.
- They decided to analyse the boys separately to the girls. I wonder if the sample had been combined whether the statistically significant difference would have “washed out”.
When I calculated the 95% confidence intervals of the data, I found that these were very wide and this is a reflection of the small sample size. This illustrates that we cannot have confidence in the data concerned with the differences that they detected.
It is also relevant to point out that this paper is consistently misquoted, for example, I have taken this quote from a paper published a few years later
“Linda Aronson has shown that the direction of mandibular growth measurement at gnathion was more horizontal following adenoidectomy and a change in the mode of breathing”.
While I know that I have been critical of this paper, I also wonder if there is trend in the data. In this respect, it is a shame, that all these years later, a trial has not been carried out to attempt to answer this question.
I have reviewed the Cochrane library for additional information and come across several reviews that provide us with useful information on breathing, sleep disordered breathing and their treatments. I will follow this post up to discuss these papers and perhaps we could come to some conclusions about the current interest in breathing and orthodontics.

Emeritus Professor of Orthodontics, University of Manchester, UK.
Devil’s advocate:
Whether mouth breathing is related to orthodontics is irrelevant given the consequences of upper airway obstruction in kids in the first place
There are orthodontists of prominence telling parents not to have ENT procedures because the evidence indicates it makes difference to the jaw and teeth. And one of these is a prominent researcher and university lecturer.
In my mind this advice is unethical and misinformed.
http://www.slideshare.net/AssocProfDavidMcInto/mouth-breathing-58269960
Could you be more specific? I’m trying to wrap my mind around which ENT procedures a prominent ortho would not want done.
Adenoidectomy
Tonsillectomy
Turbinate reduction
I am very interested in finding out what is new in this area. I have a strong sense that there is a relationship, but of course, that is not very scientific. Thanks for reviewing.
How can you have your pudding if you don’t eat your meat?
I think there is a sequence of things to look into here – we had a guy down to the IDA last year talking about perio disease and systemic (especially cardiac) illness. The premise was this:
1 You can investigate something that you think will be connected because you can demonstrate a series of known phsiological phenomena that in theory could be connected
2 You then look for an association between A and B
3 You then see if treating A has an effect on B
So for ortho and nasal breathing, there must have been:
1 some guy that could have conjectured ” mouth breathers are more likely to have ortho problems and here’s why” before anyone did any clinical studies.
2 Then there should have been a guy that demonstrated that mouth breathers did indeed have these problems- I am thinking here of epidemiological sized samples, comparing mouth breathers to controls/nasal breathers
3 And then, when you have some progress with 1 and 2, you put together a study to treat the mouth breathing and see if it affects the ortho problem.
Now, this paper you describe looks like an attempt at number 3, but I would like to know who are the legit researchers are for 1 and 2 above?
I went through post grad ortho largely given the impression that breathing makes no huge difference to maloccusions. Then mixing with postgrads from other countries, I discovered this isn’t necessarily the prevailing opinion outside the UK. But when I moved into practice in the Adenoid Belt of the Nasal-congestion Nebulae, I see stacks of kids with high angles and molar crossbites and low overbites. Cause and effect, chicken and egg, I don’t know, but I would be interested in legit statistics to see if I am just imagining the connection.
As for ENT intervention causing an improvement in the Ortho, that has got to be age sensitiven if it happens at all. As for ortho intervention improving the ENT – that has got to be the new frontier.
Most of the original papers come from the 1920s. As best as I can tell, Alfred Paul Rogers was one of the leaders in the field. These papers are still available online.
ENT helping ortho- the papers show the best outcomes come about in kids having ENT problems sorted before age 6.
You might find it helpful to research papers on kids with allergic rhinitis and malocclusion- 3-4x more prevalent in those kids with allergies
The problem with this study, as I recall, is that the authors–during discussions and presentations–were unable or unwilling to acknowledge a difference between statistical significance (which was marginal) and clinical significance. The explained variance was minimal.
Do ENT surgeons do as many adenoidectomies as they used to? I was under the impression that (like grommits) they had stopped doing it quite so often since most adenoid related problems go away with time and growth, in which case maybe orthodontists who advocate early treatment for breathing problems may have just re-invented an unecessary treatment for a non-problem.
Is there an ENT consensus on this?
Financial success in 3 easy steps: 1) invent a disease, 2) specify “diagnostic” criteria that say everyone is sick, and 3) treat the disease, secure in the knowledge that your salable treatment is so irrational that it will never be tested and thus will matter only to your bottom line. Is this a great calling, or what?
“Don’t be afraid to care” PF
Acute acrylic insufficiency syndrome?
Are there any position papers from ENT societies pro/con on the topic?
Is maxillary expansion enough or is soft tissue reduction further posterior also needed?
This is a classic paper of wrong statistics leading to wrong conclusions. The figure to note is Figure 4: observe the two female outliers at the far left of the graph. It is obvious that the distribution of adenoidectomy cases is not normal. If these two outliers are removed then the difference is not statistically significant anymore (I run a t-test using approximate values obtained from the graph). I also tried a Mann-Whitney test, with outliers included, and the result was not statistically significant. It is interesting that the authors report a statistically significant difference in variances between the control and adenoidectomy groups, yet they carried out t-tests instead of non-parametric tests. Observe also that Figure 4A shows 14 females in the adenoidectomy group, instead of the 16 reported in the text and Table II.
I understand that the paper was published back in 1986, but it seems that it still influences our thinking on this important subject. Would we accept this paper for publication today?
Look around and choose your own ground:
Why not a prospective breathing study using RPE? As orthodontists, this is our ground.
Yes, and this would not be difficult to do. I think that the proponents of these techniques should carry out this research
looking forward to the next part!