Evidence based orthodontic treatment-no good deed goes unpunished.
Evidence based orthodontic treatment-no good deed goes unpunished.
In September Professor Lysle Johnston and I did a joint presentation at the British Orthodontic Conference with a focus on evidence based orthodontic treatment. We have decided to write this up as two blog posts. I have based the first of these on my presentation.
 Uncertainty, evidence and patient decision aids
Uncertainty, evidence and patient decision aids
Uncertainty is present in all aspects of our lives. This is particularly true for all our clinical decisions. We can never be 100% certain about our treatment. One way of reducing clinical uncertainty is to carry out research and incorporate this evidence into our decisions. Paradoxically, claims about treatments, based on low levels of evidence, increase clinical uncertainty.
We may all be familiar with the pyramid of clinical evidence. This classifies research methods that have the potential to reduce uncertainty. But this is not the whole story. We must remember that in order to practice evidence-based care, we must also consider clinical experience and patient’s opinion. Importantly, when evidence is absent, clinical experience is important. But we should remember that when research evidence is strong this should outweigh the role of clinical experience. I have posted about this before.
There have been many trials carried out into orthodontic treatment and we are starting to establish a strong evidence base. Unfortunately, I am not sure that we are translating this evidence into practice. I also wonder if we are not explaining this research to our patients so that they can take informed decisions on their care. One solution to this is a relatively new concept of patient decision aids. These are documents or computer-based programs that are designed to inform people about the evidence. Recently, a team from Sheffield, UK has published an very interesting study on an orthodontic decision aid. I’m going to post about this in a couple of weeks.
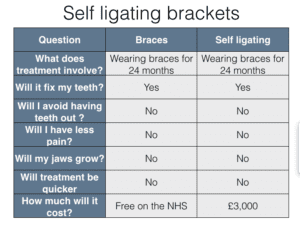
I have illustrated this concept by quickly putting together a basic patient decision aid developed from the evidence on self ligating brackets. This is just an illustration, but I can see that this approach could be very useful.
Can we reach this orthodontic nirvana?
In theory, I hope that this is the start of an orthodontic nirvana with us all working together to help our patients take decisions. But I do worry that this is not the case because of unsubstantiated claims that are being made about types of treatment.
I also find it very interesting that this promotion of untested treatment is effective. In fact, I wonder if the promotion is more effective than the treatment! As a result, I have investigated the concept of uncertainty a little further. My main source has been two books on uncertainty in the way that we think (Nowotny and Kahneman). In brief, it appears that humans struggle to think statistically and we do not like chance. Yet our lives are full of uncertainty. Finally, one of the main problems with the dissemination of research is that uncertainties are couched in precise, yet cautious terms. This is illustrated by these two quotes. This first one is by me.
“When functional appliance treatment is provided in early adolescence it appears that there may be minor beneficial changes in skeletal pattern, however, these are probably not clinically significant”.
I have taken the second one from a website on orthotropic treatment
“There is also evidence to suggest that improving the health and shape of the face reduces jaw joint problems, upper neck and back problems, speech problems, and most ENT problems, such as sinusitis, glue ear and middle ear infections. Children and adults with healthy, functioning faces enjoy lifelong benefits, including all those that come with a confident, beautiful smile”.
When you look at these two statements it is clear that the more compelling is the latter, as it is more certain. Yet, in my opinion, it is not supported by research evidence.
Are there solutions?
What is the solution to this problem? I cannot help feeling that this is more easily said than done. In short, we need to educate. This means that we need to explain research findings in a more understandable way and not always confine our methods of dissemination to complex articles in the journals. We also need to educate specialists and dentists in how to interpret research findings. Finally, we need to adopt the methods used in social media to inform our patients of the evidence that underpins their treatment. These are challenges that we need to address.
The second part of this post will be by Lysle Johnston, when he will discuss the role of the randomised trial in orthodontic research.

Emeritus Professor of Orthodontics, University of Manchester, UK.
Kevin
really enjoyed yours and Lyle’s presentations at confence, and great you are writing them up
IMHO the problem is the way dentistry is taught at undergrad level – we (as teachers) no not challenge students to question us or the evidence on which clinical decisions are based. Too much is ‘that my way’ rather than what is the ideal for this patient based up the evidence and clinical situation. Hence IMHO why too many dentist do not question the evidence for PR hype
Kevin, Lysle,
I find it sad that the tolerance we have for others to express opinions is abused by people arguing against strong evidence. When their arguments are the existing hypothesis, which continues to fail to support their favorite approach, their attitude is the research got it wrong, classical Kahneman ‘fast thinking’.
We have had recent verification of the deficiencies of NHST and p-values by the American Statistical Association but the material presented by the pseudo-scientists is often hearsay and case reports, a denial of the weaknesses of fast thinking.
I give the example of Professors who will recite the results of RCTs which show predominant dento-alveolar change with Class II treatment alone with intra-oral mechanics from say inter-arch elastics compared to a ‘functional’ appliance and then suggest that despite both approaches yielding almost indistinguishable change they then propose an illogical leap, they say one approach being able to avoid extractions or produce a differing result. Sadly, such an attitude denies the results they champion.
We need to trust and live our science stats and follow through to speak out over false claims of efficacy. The public deserves to have the best information provided to them. We further, need to vigorously dismiss long standing claims that are at odds with research results.
People don’t think statistically because they have strong emotional drive for success. Humans are wired to use their emotional responses when they need to assess complex problems that have multiple, indeterminate features. (Like Orthodontics). This explains to me why one finds so much snake oil gets sold in orthodontics. Our orthodontic environment is often too complex to reduce to simple A-B comparisons. So, Hope and Desire – that are very powerful drives in humanity – will step in to bias un-trained viewpoints. Whether we are testing new treatments or assessing claims about snake oil – its the same.
It takes a lifetime of rigourous and devoted training in science to overcome objective bias. Remember how much value “being like others” and the “power of success” has in social environments.
I believe that our problem is that since orthodontics became a profession, more than 100 Y ago, its main problem remain Class II malocclusion where the mandible is retrusive. Every few years somebody comes with a great idea. A new appliance is being presented to the profession, and the inventor begins his wourld wide round or tour, giving lectures with phenomenal results. When I say phenomenal I do mean it! The echo this inventor leaves is amazing. The rush to its new appliance that get all the imaginable and unimaginable superlative becomes the one that most peofessionals are using. Unfortunately the reality is not so promising and slowly slowly the new invention is being abandoned and the profession is waiting fir the new savior and so on. Nobody is looking for the basic evidence based publications and the self experience is the winner. I know that this will go on and on as it went on and on. The eagerness to solve all kinds of problems is growing. This is unfortunately a never ending story…
Kevin, I am not sure education of dental specialists, i.e., orthodontists is an answer since I see them abandon almost everything they have learned in their specialty training to endorse specious theories and use them in therapy.
As I posted earlier (but did not make the posting board ) I find PSL giving me better faces ,faster tmnt.much less EXTN. etc.etc.
I am really confused ,as I value greatly the academic input, but how am I seeing this ? Am I missing something ?How can I go from 30% extn. to 5% by using PSL.My clinical findings don’t jibe with your research findings and that of others.Kindly help me understand this
Hi Andrew; It is an example of observer-expectancy effect which even with RCT’s is difficult to reduce this potential source of bias unless it can be blinded somehow. I see great faces with my non-SL brackets – some are extraction, most are non-extraction. I have also made occasional errors (in my opinion) by extracting in some cases and not extracting in others. There are many inefficiencies in some treatment protocols and just making small changes can significantly reduce treatment times (e.g. wire sequences, appointment intervals, and choosing non-extraction over extraction). However, when you focus on the one component (i.e. the bracket) you assume any improvements are due to that one factor. Orthodontics in the USA had an extraction rate of 6.5% in 1913 (with bands on every tooth) but was 80% by 1966 and both were influenced mainly by individuals with compelling personalities and demonstrating nicely treated cases by the standards of that time (biased source of low-level evidence). The USA average now sits around 15% (JCO) but Angle (and Old Glory) would have considered your 5% ‘extractionist’ which really is just a matter of perspective. In a survey I conducted in Australia in 2013 the extraction rate varied from 4% to 80% and both individuals probably consider the other one to be wrong (the median was ~20%). However there are a large number of well-designed prospective RCT’s finding no difference – some are extraction studies, some are non- or both. This data is quite compelling that there is no advantage. I have used ASL, PSL and conventional and my experience is that I prefer conventional. However with your clinical experience you find it suits your diagnosis and treatment protocol then use it by all means.
Peter -Thankyou so much for your well thought out comments ! I totally agree there is no magic bracket ! I think it is the combination of PSL,modern/ advanced wires ,early elastics etc. etc. that made the huge differences in my life ie. the system as a whole.
For example ,in essence ,faster tmnt.better outcomes ,less stress in my office and better financials .I come from 35 yrs of practice and experience ,hopefully not 1 yr of experience repeated 35 times !
Again ,appreciate the science and comments,love the paper critiques —keeps me on my toes !
Sorry to add to the repeated flogging of this horse!
Dear Prof O’Brien,
It is my understanding based on the science at hand we now have as much evidence for Orthotropic growth correction as we do in Orthodontics as an entire discipline.
Orthotropics is defined as correcting growth and it derives its changes from postural forces. It is unlike functional orthodontics which relies on functional forces. William Proffit was very clear in his Equilibrium Theory, functional forces are heavy and short, postural forces light and long. Functional forces move us physically in space while postural forces move us biologically in adaption.
All functional appliances whether they be fixed as Jasper Jumper or removable Twin Block or Frankels have been proven to be useful for dentoalveor changes but little else. Your work amongst others provided this evidence.
Orthotropic forces are light and continuous, these (penalty provoking) appliances condition the voluntary change to a closed mouth resting posture. It is this long and light uplifting from increased and controlled muscle tone that stimulates biological change through the associated basal bone.
Mandall’s 2016 Class III protraction facemask RCT trial clearly showed growth related changes with long term, light and continues forces applied to the maxilla. Your comments: “A real Landmark”, “An excellent study that the authors carried out reported very well.”, “It’s findings will change practice.”
Conversely for evidence to support Orthotropic therapy in general, the Millet, O’Brien 2006 (revised 2012) Cochrane Collaboration was equally definitive. “It is not possible to provide any evidence based guidance to recommend or discourage any type of orthodontic treatment to correct Class II division 2 malocclusion in children.”
Actually reflection of your specific comments and your authorship of perhaps the most scientific journal we have at hand, we actually have more evidence basis for treating with Orthotropics than we do our daily practice of Orthodontics.
Regards,
Simon Wong
Dear Prof O’Brien,
It is my understanding based on the science at hand we now have as much evidence for Orthotropic growth correction as we do in Orthodontics as an entire discipline.
Orthotropics is defined as correcting growth and it derives its changes from postural forces. It is unlike functional orthodontics which relies on functional forces. William Proffit was very clear in his Equilibrium Theory, functional forces are heavy and short, postural forces light and long. Functional forces move us physically in space while postural forces move us biologically in adaption.
All functional appliances whether they be fixed as Jasper Jumper or removable Twin Block or Frankels have been proven to be useful for dentoalveor changes but little else. Your work amongst others provided this evidence.
Orthotropic forces are light and continuous, these (penalty provoking) appliances condition the voluntary change to a closed mouth resting posture. It is this long and light uplifting from increased and controlled muscle tone that stimulates biological change through the associated basal bone.
Mandall’s 2016 Class III protraction facemask RCT trial clearly showed growth related changes with long term, light and continues forces applied to the maxilla. Your comments: “A real Landmark”, “An excellent study that the authors carried out reported very well.”, “It’s findings will change practice.”
Conversely for evidence to support Orthotropic therapy in general, the Millet, O’Brien 2006 (revised 2012) Cochrane Collaboration was equally definitive. “It is not possible to provide any evidence based guidance to recommend or discourage any type of orthodontic treatment to correct Class II division 2 malocclusion in children.”
Actually reflection of your specific comments and your authorship of perhaps the most scientific journal we have at hand, we actually have more evidence basis for treating with Orthotropics than we do our daily practice of Orthodontics.
Regards,
Simon Wong
Thanks for the comments. I think that your viewpoint is a really statement on how you can quote and interpret the scientific literature to suit your views. I am not sure how much orthodontic research you have read but it is my view that there is more good orthodontic research on the effects of treatment than I have seen for orthotropics. In fact I have not seen a single good research paper on orthotropics. I keep asking for them but no one can suggest one. Have you any that you could let me have the references for?
RE Peter Miles comments which are much appreciated and valid and to reflog this ,already heavily flogged horse ; I believe the PSL bracket is just one component of the PSL system ie. early elastics ,longer time between appts ,non -extn,more advanced wire material etc. etc. All this and more has revolutionized the outcomes ,stress level and financials in my practice .BUT ,still appreciate the great comments on the research—keeps me on my toes!!
Meta-physical
In our quest for direction
we seek evidence in purpose
and when this base is weak
we search for answers from within
standing still at this clinical crossroad
amidst science that lies scattered
soon we look towards ourselves
and also our patients
for signs and meaning, so-called expertise
for the road ahead
Instead let us now seek
neither from our own, nor of our own
for the way ahead
lies away from such comforts
and the way forwards
resides in the universal realm
where knowledge unites
gathering and collecting
evidence and wisdom
seek we must
with a purity in pursuit
an interest in quest, metaphysical
from this will dawn
new evidence and knowledge
revealing the truth
the collective fruit of labour
that is for the best of our science
that is for the best for our patients’
Prof O’Brien,
Mew J 2007, Facial changes in identical twins treated
by different orthodontic treatments. World Journal of Orthodontics.
Mew J 2016, Visual comparison of excellent orthodontic results with excellent postural results. Kieferorthopaedia.
Gibbs W 2014, The effect on the adult face of different orthodontic techniques in different ages. Journal of Gnathologic Orthopaedics and Facial Orthotropics.
Singh G 2007, Evaluation of the posterior airway space following Biobloc therapy: Geometric morphometrics. Journal of Craniomandibular practice.
Singh G 2009, Soft tissue changes using Biobloc appliances: Geometric morphometrics. International Journal of Orthodontics.
Trenouth M 2001, A cephalometric analysis of the Biobloc technique using matched normative data. Journal of Orthofacial Orthopaedics.
I absolutely agree the level of research on Orthotropics is abysmal. And yet there is nothing that disproves it because almost all the research we have is in functional appliances and not postural ones?
But please do explain to me why after 100 years of science we have only one robust RCT study on the effectiveness of protraction as a mode of therapy in Class III patients and no RCT studies on even how to effectively treat Class II Div2 malocclusion?
Is my logic not correct for maxillary protraction appliances, that they use long and light forces, a postural force ? Are other functional orthodontic appliances predominately functional ones that act mostly when we open our mouths in functional mal movements ? Could it be that for large scale change functional forces are ineffective but postural forces do create change?
I read your Cochrane paper. The literature in 2006 for evidence based science in our profession was non existent. When you reviewed it again 2012 nothing had changed. Is it any better now in 2017? Are we any closer to having an evidenced based recommendation for possibly the single largest malocclusion in all our practices?
If not, why not?
Is it possible that vigorous, robust studies are actually extremely difficult to do in orthodontics? Possible only in institutional settings and not really the relmn of the common every day wet handed clinicians?
Only Professors of major Universities have the capacity to commission decent studies. You are amongst this elite small number of people who have influence.
The Millet paper revealed a large gap in our science in 2006. Unless I’m mistaken you were a lead author in this? In the last 10 years, what has actually changed? What, as a person of enormous research resource, have you done to rectify this bizzare blight in our profession?
I cannot in my right mind believe you would accept this deficiency and move on. I do believe and readily accept this is a true reflection of how nearly impossible it is to prove what is it we do in our practices.
Is more research being done for Class II div2 malocclusion and about to be released but we are not yet aware of? If not and if we are actually interested in being an evidence based scientific profession, is this not worth a more detailed response than a brush off comment?
Regards,
Simon
Hi Simon, thanks for the comments. I did not mean to brush you off.
Firstly, thanks for the list of papers. They are all case series or restrospectice studies and are generally low levels of evidence. They certainly do not provide information that is sufficient to change practice.
When I look at your other comments. There are several studies on Class II malocclusion and they provide us with good evidence which does not support any of the concepts on orthotropics.
I agree that there is only one study on Class III and this was good. But I would not say that the forces are light, so I do not follow your logic.
I agree that we do not study Class II div 2 much and there is a need to do this research.
Most studies are carried out in universities and this does influence generalisabilty.
You ask what I have done since I carried out the research that you have quoted. I have continued to do some research, but I have been the Dean of a Dental School, then Aasociate Dean of a Faculty, then Chair of the General Dental Council. I have now returned to research work as the Director of a clinical trials unit. This involves supporting clincical trials in medicine, surgery and cancer. All fields that demand high levels of evidence. Unlike some parts of orthodontics where people adopt alternative method with no critical thought turning a blind eye to studies that do not support their confused beliefs. All I want to see is one decent study on orthotropics……
Dear Prof O’Brien,
I do appreciate your detailed response as you clearly have many duties and responsibilities. Thank you.
With regards to the forces on the maxilla in the Class III protraction, the term is relative as we are not discussing teeth but rather basal bone structures. What is light on an individual tooth is miniscule against the maxilla. What is still considered light on the maxilla, may be impossibly heavy on a tooth. That said, the continuous nature of forward pull protraction, in relative terms still constitutes a postural rather than a functional force. My assumption of course with facemask protraction we are not trying to split any sutures (that would require a functional force) but to stimulate remodelling and or growth trend changes.
Mandall’s study clearly reveals skeletal (and more than the typical dentoalveolar) changes from an environmental force rather than any innate genetic growth pattern. Again these are all ideas encompassed by the Orthotropic Tropic Premise and throws an interesting light on the pure genetics campers. This study surely highlights the need for much more research in the aetiological basis of malocclusion!?
Sadly in all other matters I agree with your views. Too much we tout our wares without the consistent delivery of tangible goods. With your influence I am certain more trials will be commissioned to solidify the science of orthodontics. Personally I hope to play my part in correcting this particular oversight in Orthotropics.
Shortly I plan to begin the process of adding to the research base for Orthotropics. As we discussed in previous correspondence I have almost completed and comprehensively documented 10 Orthotropic cases including before and after Cephalometrics but will delay until 2017 to present you. Orthotropics is a long process with a 3-4 year timeline so collecting full records on these cases draws out the process further. Also I wish to have two dozen cases to submit to you so as not to appear to be misrepresenting by “cherry picking”.
Further more we are fortunate enough to also be supervising the commencement of 10 new Orthotropic cases in the Orthodontic programme at Valencia University. In a few years we will be able to present more than just my own practice records and begin the process of putting to rest the misconceptions that shroud our work.
Regards,
Simon
Hi Simon, thanks. It is really good to hear that someone is prepared to try and carry out some research into orthotropics. You are probably the first person who is prepared to do this. I am a little confused that you feel the need to delay showing the results for a couple of years. why not show them now and then again later?
Best wishes Kevin
thanks for the article. I disagree slightly with the table comparing Self Ligating and conventional brackets. They are essentially the same except that Conventional Braces are Free on NHS and self ligating cost £3000. If a practitioner used self ligating brackets on his NHS patients (and I know a few that do) then they would also be free. If a practitioner used conventional braces on his private patients, they could also cost £3000 or whatever his fee was. I don’t think the choice of bracket determines the entitlement to NHS treatment. It may have a bearing on the practitioner’s expenses and their enthusiasm to provide the treatment privately or under the NHS, but you could say the same about ceramic brackets.