Maxillary Expansion with skeletal anchorage explained: MSE vs Hybrid Hyrax
This is a guest post by Benedict Wilmes. I was confused about the differences between RME, Hybrid Hyrax, MARPE, and MSE expansion. As he is a world expert on mini-implants, I asked him to help me. As a result, he wrote this great short blog post, with an extensive list of references. I now understand and I hope that you find it useful.
Introduction
Maxillary transverse deficiency is a common orthodontic problem. It is often associated with a unilateral or bilateral posterior crossbite. Rapid maxillary expansion (RME) is considered the optimal procedure to achieve skeletal widening of the maxilla.1,2 Since the anchor teeth distribute the forces to the bony structures via the anchor teeth, distribution of the forces to as many teeth as possible and completion of root growth are considered essential. However, side effects, for example, tipping teeth, root resorption, decrease in buccal bone thickness or dehiscence, and loss of marginal bone height resulting in gingival recessions may occur.3-6
Mini Implants in expansion appliances
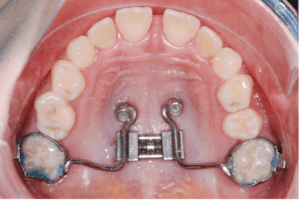
More recently, we have used mini-implants to share the load of the expansion with the anchorage teeth to reduce or eliminate the unwanted dental side effects. Wilmes et al. introduced the Hybrid Hyrax expander in 2007 using two mini-implants in the anterior palate and two (deciduous) molars (Fig. 1).7-10
Similar hybrid expanders were published in the following years by Garib11 in 2008, Lee12 in 2010, and Moon13 in 2015 called MSE (Fig. 2, Mini-Screw Assisted Expansion).

Mini-implant-supported expanders can be used very successfully to treat growing Class III patients14-21 allowing skeletal maxillary protraction without the common dental side effects.13,16,17,22. Additionally, alternating expansion and constriction of the maxilla Alt-RAMEC21,23 over nine weeks can enhance the response of the maxilla to the protraction forces and offer a good response in children with more sutural maturation.24-26
TAD insertion sites
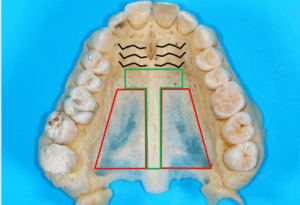
For the stability and predictability of the mini-implants (TADs), we need to place them in the areas with the best cortical bone quality. Several CBCT studies have shown that this is in the anterior palate along an area designated as the T-Zone (Fig. 3).27-29
In the conventional Hybrid Hyrax, the mini-implants are placed paramedian in the anterior palate in the T-Zone. An impression or scan is taken and sent to a laboratory to manufacture the appliance, which is then fitted in a subsequent appointment. More recently, we can make these appliances using selective laser melting procedures.30 The available printing metal powders provide a high rigidity of the appliance, which seems very important, especially for expansion appliances. Furthermore, we can make this process more efficient using CAD/CAM manufactured insertion guides, which facilitate a safe and precise insertion of mini-implants in the anterior palate in the areas of the best bone. Importantly, these insertion guides allow for the insertion of mini-implants and installing the appliance in a single appointment.31,32
TADS first approach
In both of the above approaches, with impression/scan and insertion guides, mini-implants are inserted first, and the appliance is installed afterward. This method can be called “TADs First”. A disadvantage of this “TADs First” procedure is the need for two appointments. One to insert the TADs and the second to cement the appliances. Using the insertion guide eliminates this issue, however. Secondly, the appliances may not fit if there are inaccuracies during the manufacturing process. This problem may also occur when using an insertion guide, especially if there is a change due to tooth eruption or movement from the original scan to the insertion appointment.
Appliance first approach
As an alternative to the TADs First concept, it was proposed to insert the expansion appliance first and 2-4 mini-implants afterward. For example, with the MSE.33 This protocol can be called “Appliance First”. A disadvantage of the conventional appliance first method is choosing the placement site for the mini-implant freely based on bone quality. The prefabricated nature of the appliance restricts the placement site of the mini-implants. It may be possible to shift the mechanisms forwards or backward to allow the channels to line up with an area of good bone. Unfortunately, it is unlikely that all 2-4 mini-implants will be consistently in the best bone quality areas. This problem is especially pertinent in the posterior molar area where the bone height is only 1-2 mm in paramedian sites.27,34 Additionally, the connection between the expander and the mini-implants in those appliances is not rigid and angularly stable. As a consequence, mini-implants have some play with the expander and will tip as soon as the expander is activated.35
Pros and Cons of “Appliance First” method versus “TADs First” method
Advantages of the “Appliance First” method (MSE):
- Mini-implant insertion and installation of the appliance in just one appointment.
- No impression/scan is needed after mini-implant insertion
- No risk for a misfitting of the appliance and the mini-implants
Advantages of the “TADs First” method (Hybrid Hyrax):
- The appliance can be removed and re-installed easily, for example, for modifications or repairs.
- Rigid and stable connection between the mini-implants and the expansion appliance
- The customized design allows total freedom in selecting the mini-implant sites to utilize the best available bone.
- Mini-implants can be used to anchor more than one appliance, for example in the first step for rapid maxillary expansion and in a second step for molar distalization.36
References
- Kurol J, Berglund L. Longitudinal study and cost-benefit analysis of the effect of early treatment of posterior crossbites in the primary dentition. Eur J Orthod 1992;14:173-179.
- Camacho M, Chang ET, Song SA, Abdullatif J, Zaghi S, Pirelli P et al. Rapid maxillary expansion for pediatric obstructive sleep apnea: A systematic review and meta-analysis. Laryngoscope 2017;127:1712-1719.
- Garib DG, Henriques JF, Janson G, de Freitas MR, Fernandes AY. Periodontal effects of rapid maxillary expansion with tooth-tissue-borne and tooth-borne expanders: a computed tomography evaluation. Am J Orthod Dentofacial Orthop 2006;129:749-758.
- Schuster G, Borel-Scherf I, Schopf PM. Frequency of and complications in the use of RPE appliances–results of a survey in the Federal State of Hesse, Germany. J Orofac Orthop 2005;66:148-161.
- Erverdi N, Okar I, Kucukkeles N, Arbak S. A comparison of two different rapid palatal expansion techniques from the point of root resorption. Am J Orthod Dentofacial Orthop 1994;106:47-51.
- Akyalcin S, Alexander SP, Silva RM, English JD. Evaluation of three-dimensional root surface changes and resorption following rapid maxillary expansion: a cone-beam computed tomography investigation. Orthod Craniofac Res 2015;18 Suppl 1:117-126.
- Wilmes B, Drescher D. A miniscrew system with interchangeable abutments. J Clin Orthod 2008;42:574-580; quiz 595.
- Wilmes B. Fields of Application of Mini-Implants. In: Ludwig B, Baumgaertel S, Bowman J, editors. Innovative Anchorage Concepts. Mini-Implants in Orthodontics. Berlin, New York: Quintessenz; 2008.
- Wilmes B. Anwendungsgebiete von Mini-Implantaten. In: Ludwig B, editor. Mini-Implantate in der Kieferorthopädie – Innovative Verankerungskonzepte. Berlin: Quintessenz; 2007. p. 89-120.
- Wilmes B, Nienkemper M, Drescher D. Application and effectiveness of a mini-implant- and tooth-borne rapid palatal expansion device: the hybrid hyrax. World J Orthod 2010;11:323-330.
- Garib DG, Navarro R, Francischone CE, Oltramari PV. Rapid maxillary expansion using palatal implants. J Clin Orthod 2008;42:665-671.
- Lee KJ, Park YC, Park JY, Hwang WS. Miniscrew-assisted nonsurgical palatal expansion before orthognathic surgery for a patient with severe mandibular prognathism. Am J Orthod Dentofacial Orthop 2010;137:830-839.
- Moon W, Wu KW, MacGinnis M, Sung J, Chu H, Youssef G et al. The efficacy of maxillary protraction protocols with the micro-implant-assisted rapid palatal expander (MARPE) and the novel N2 mini-implant-a finite element study. Prog Orthod 2015;16:16.
- Wilmes B, Nienkemper M, Ludwig B, Kau CH, Drescher D. Early Class III Treatment with a Hybrid Hyrax-Mentoplate Combination J Clin Orthod 2011;45:1-7.
- Stocker B, Willmann JH, Wilmes B, Vasudevan S, Drescher D. Wear-time recording during early Class III facemask treatment using TheraMon chip technology. Am J Orthod Dentofacial Orthop 2016;150:533-540.
- Nienkemper M, Wilmes B, Franchi L, Drescher D. Effectiveness of maxillary protraction using a hybrid hyrax-facemask combination: A controlled clinical study. Angle Orthod 2015;85:764-770.
- Ngan P, Wilmes B, Drescher D, Martin C, Weaver B, Gunel E. Comparison of two maxillary protraction protocols: tooth-borne versus bone-anchored protraction facemask treatment. Prog Orthod 2015;16:26.
- Wilmes B, Ngan P, Liou EJ, Franchi L, Drescher D. Early class III facemask treatment with the hybrid hyrax and Alt-RAMEC protocol. J Clin Orthod 2014;48:84-93.
- Baccetti T, McGill JS, Franchi L, McNamara JA, Jr., Tollaro I. Skeletal effects of early treatment of Class III malocclusion with maxillary expansion and face-mask therapy. Am J Orthod Dentofacial Orthop 1998;113:333-343.
- Jager A, Braumann B, Kim C, Wahner S. Skeletal and dental effects of maxillary protraction in patients with angle class III malocclusion. A meta-analysis. J Orofac Orthop 2001;62:275-284.
- Foersch M, Jacobs C, Wriedt S, Hechtner M, Wehrbein H. Effectiveness of maxillary protraction using facemask with or without maxillary expansion: a systematic review and meta-analysis. Clinical oral investigations 2015:1-12.
- Ngan P, Moon W. Evolution of Class III treatment in orthodontics. Am J Orthod Dentofacial Orthop 2015;148:22-36.
- Liou EJ. Effective maxillary orthopedic protraction for growing Class III patients: a clinical application simulates distraction osteogenesis. Prog Orthod 2005;6:154-171.
- Buyukcavus MH. Alternate Rapid Maxillary Expansion and Constriction (Alt-RAMEC) protocol: A Comprehensive Literature Review. Turk J Orthod 2019;32:47-51.
- Franchi L, Baccetti T, Masucci C, Defraia E. Early Alt-RAMEC and facial mask protocol in class III malocclusion. J Clin Orthod 2011;45:601-609.
- Almuzian M, McConnell E, Darendeliler MA, Alharbi F, Mohammed H. The effectiveness of alternating rapid maxillary expansion and constriction combined with maxillary protraction in the treatment of patients with a Class III malocclusion: a systematic review and meta-analysis. J Orthod 2018;45:250-259.
- Becker K, Unland J, Wilmes B, Tarraf NE, Drescher D. Is there an ideal insertion angle and position for orthodontic mini-implants in the anterior palate? A CBCT study in humans. Am J Orthod Dentofacial Orthop 2019;156:345-354.
- Kang S, Lee SJ, Ahn SJ, Heo MS, Kim TW. Bone thickness of the palate for orthodontic mini-implant anchorage in adults. Am J Orthod Dentofacial Orthop 2007;131:S74-81.
- Wilmes B, Ludwig B, Vasudavan S, Nienkemper M, Drescher D. The T-Zone: Median vs. Paramedian Insertion of Palatal Mini-Implants. J Clin Orthod 2016;50:543-551.
- Graf S, Cornelis MA, Hauber Gameiro G, Cattaneo PM. Computer-aided design and manufacture of hyrax devices: Can we really go digital? Am J Orthod Dentofacial Orthop 2017;152:870-874.
- De Gabriele O, Dallatana G, Riva R, Vasudavan S, Wilmes B. The easy driver for placement of palatal mini-implants and a maxillary expander in a single appointment. J Clin Orthod 2017;51:728-737.
- Wilmes B, Vasudevan S, Drescher D. CAD-CAM-fabricated mini-implant insertion guides for the delivery of a distalization appliance in a single appointment. Am J Orthod Dentofacial Orthop 2019;156:148-156.
- Carlson C, Sung J, McComb RW, Machado AW, Moon W. Micro implant-assisted rapid palatal expansion appliance to orthopedically correct transverse maxillary deficiency in an adult. Am J Orthod Dentofacial Orthop 2016;149:716-728.
- Kang S, Lee SJ, Ahn SJ, Heo MS, Kim TW. Bone thickness of the palate for orthodontic mini-implant anchorage in adults. Am J Orthod Dentofacial Orthop 2007;131:S74-S81.
- de la Iglesia G, Walter A, de la Iglesia F, Winsauer H, Puigdollers A. Stability of the anterior arm of three different Hyrax hybrid expanders: an in vitro study. Dental Press J Orthod 2018;23:37-45.
- Nienkemper M, Pauls A, Ludwig B, Wilmes B, Drescher D. Multifunctional use of palatal mini-implants. J Clin Orthod 2012;46:679-686; quiz 703-674.

Emeritus Professor of Orthodontics, University of Manchester, UK.
Very,very helpful.Thankyou .
This is a very useful summary and I would like to thank Prof Wilmes for this work. Thinking more broadly, one has to be wary of the “treatment as a foundation” approach vs. “diagnosis as a foundation” approach. Altho’ this article deals with transverse maxillary deficiency, others in our profession are interested in nasal floor width to address diagnoses associated with sleep disordered breathing. This is one reason why clinicians wanted to move away from devices with dento-alveolar effects primarily to those that target the palatal deficiency more specifically. In addition, someone needs to address the elephant in the room (in fact, there are two). The first one is clinically-obvious; the precipitation of a significant (up to 8mm) midline diastema. This requires thorough orthodontic correction post-operatively. Second, since the mechanics of these devices override biologic limits, often fracture of the pterygopalatine ‘suture’ is induced with concomitant reduction in volume of the pterygopalatine fossa that houses the sphenopalatine ganglion, etc. The consequences of this sequela is as yet unknown. I think this is a concise synopsis of MSE but clinical risks, benefits and alternatives need to be disclosed in each case.
“Fracture of the pterygopalatine ‘suture’ is induced with concomitant reduction in volume of the pterygopalatine fossa that houses the sphenopalatine ganglion, etc.”
Perhaps the quotes indicate this is not a true suture which I understand (at least I don’t think this is a suture, rather a bony approximation, but am more than willing to be wrong on this), however the “fracture” implies a bony catastrophic separation so not sure what one is describing here.
If one believes that there is lateral displacement of the maxilla and palatine bone (with the palatine bone’s pyramidal process in “close proximity” to the pterygoid plates of the sphenoid) then reduction in volume of the pterygopalatine fossa by this expansion implies that there is NOT equivalent displacement of the maxilla and zygoma at the maxillaryzygomatic suture (expansion of the maxilla has the zygomatic process of the maxillary butting head on into the zygoma) and displacement of the zygomaticotemporal suture else IF there was a displacement of the zygomaticotemporal suture and concomitant displacement of the maxilla’s zygomatic process and zygoma laterally there may be no change in volume of the fossa only in shape.
This of course does not touch on orbital volume distortions.
Gave an excuse to revisit skeletal anatomy.
But I don’t think there’s any lateral displacement of the maxilla, palatine bone, or zygomatic process of the maxilla. Part of the smoke and mirrors of orthodontics.
Excellent, no other words for it
This technology was WAY after my time! I used Expansion plates and Quadhelix!. Fabulous article though for those of us retirees who still love to keep up with modern Ortho techniques and discussions. It never leaves you!