Which closes spaces faster en masse or two-step retraction?
This post is about a new paper that investigated the simple question of what is the best method for extraction space closure. I thought that it was an interesting small study.
One of the most complex part of a course of orthodontic treatment is the closure of extraction spaces. This needs to be managed well and certainly increases treatment time. Indeed, I am sure that one reason for the current trend for non-extraction treatment is to avoid the complexities of space closure, as non-extraction treatments are less complicated. However, in many cases, it is necessary to “commit the crime” of extraction of premolars. When this is done, we have two main choices of the type of mechanics for space closure. These are en masse retraction when canine to canine are retracted in one step. Alternatively, we may decide to use a two-stage method where we retract the canines followed by the incisors.
I remember when I was training, we used to use the two-stage method. I was told that it was less intensive on anchorage. However, this did result in rather unsightly spaces as the canines were retracted. It then became trendy to use en masse retraction. We were sold on this because we were told that it was faster and more aesthetic. So I changed my mechanics to en masse. Surprisingly, there have been few trials of these different methods. I was, therefore, interested to see this new trial published in the open-access Angle Orthodontist. A team from Sao Paulo, Brazil, did this study. They have published a paper on part of this trial earlier this year.
Patricia Pigato Schneider et al
Angle Orthod. 2019;89:855–861 Doi: 10.2319/101618-748.1
What did they ask?
“Is en masse or two-stage retraction faster at closing orthodontic extraction spaces”?
What did they do?
They did a parallel-group RCT with a 1:1 allocation. The PICO was
Participants: Orthodontic patients older than 18 years old with bimaxillary proclination with mild incisor crowding. They had premolars extracted as part of their treatment.
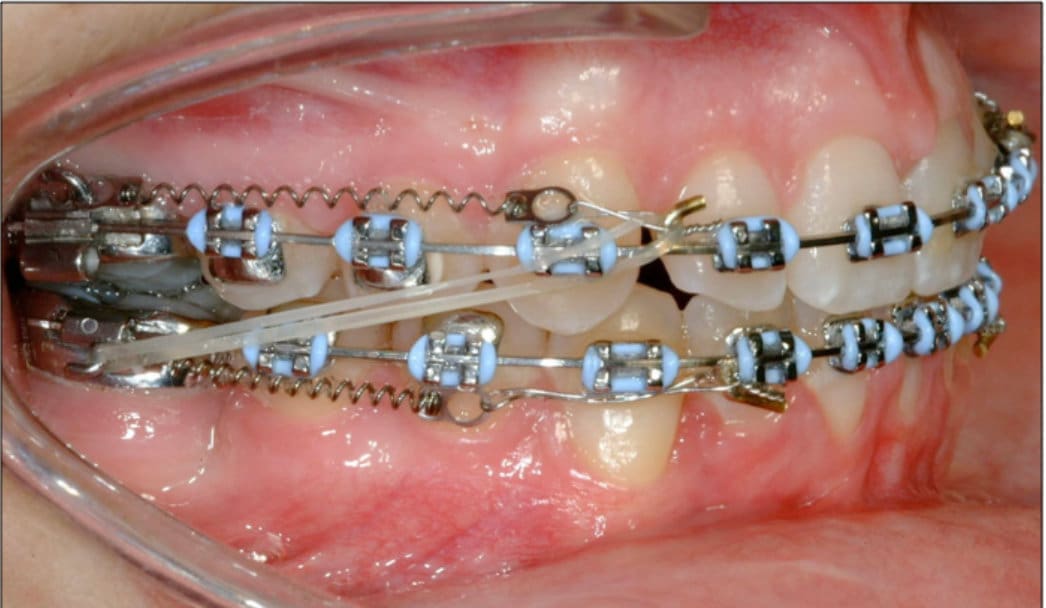
Intervention: En Masse retraction. They retracted all incisors and canines in one step. They used sliding mechanics on a 17×25 SS wire with 200g force from a NiTi closing spring. .
Control: Two-stage retraction. They fitted an 020 round SS wire with flush omega loops. They then use NITi springs with a force of 100g to retract the canines. When this was complete, they fitted 17×25 SS wires and retracted the incisors using NiTi springs with a force of 100g
Outcome: Duration of space closure.
They saw the patients every 4-5 weeks for reactivation appointments. They recorded the following information from the patients’ record.
Start of retraction (T1)
Date of completion of space closure (T2)
They then calculated the total retraction time of space closure in months.
They analysed the data with survival curves with the outcome measure of space closure time for each premolar space.
The patients were allocated to the interventions using a simple randomisation technique. I could not find any details of the method of sequence generation, concealment of allocation and blinding of examiners. I was also surprised that there was no sample size calculation. This is important, and I will come back to this later.
What did they find?
They enrolled 48 participants in the trial. All the participants completed the study.
There were no differences between the groups at baseline.
The mean time for space closure for the En Masse retraction group was 13 months (SD=0.5), and for the two-stage group, this was 25.7 months (SD=0.5). The Kaplan-Meier curves confirmed that there was a statistically significant difference between the space closure times for the two methods of space closure.
Two-stage retraction took between 1.8 and 2.2 times longer than en masse retraction.
Their overall conclusion was:
“En Masse space closure was clinically and statistically faster than two-stage retraction”.
What did I think?
This was an interesting small trial that looked at a clinically relevant question. I was very interested to see such a significant difference between the two interventions. Importantly, this difference in space closure duration may lead to similar differences in overall treatment time. I would, therefore, really like to see the total length of treatment as an outcome of this trial, and it is a shame that they did not report this.
I think that it is also essential for us to consider that the unit of analysis in this study was individual premolar space closure. While I agree that this is an important outcome. I wonder if the study would have provided us with more useful information if the authors had also presented data on the time for all space closure per patient. This would let us know the duration of the space closure phase per patient for each of the interventions.
A rant about the reporting of this study
I was surprised to see that the authors did not provide any details of the sample size calculation, sequence generation, concealment and blinding. This puts this trial at critical risk of bias. In fact, I am surprised that the referees for the journal accepted this paper without this information.
We clearly need higher refereeing standards for papers of this type. Importantly, these factors are covered in the CONSORT guidelines. The Angle has not adopted these and has not endorsed them> Whereas, the AJO, EJO and JO require authors to comply with them. Perhaps, the Angle should consider raising the standards of reporting trials by using the CONSORT guidelines?
Final comments
You may feel that I have been too critical of this study. However, we need to look at clinical studies carefully. We can then decide if we can change or continue with our practices. Nevertheless, when I consider everything, the results may be sufficient to reinforce my method of using en masse retraction.

Emeritus Professor of Orthodontics, University of Manchester, UK.
Could the anchor teeth have moved mesially more in the one stage than two stage group?
I think the authors missed the bottom line, as the criteria for choosing for one technique or the other should be the desired anchor control instead of time of treatment!!! Hopefully this will be addressed in other publication, for it is common to use different angles from the same study to multiply production.
Dr. O’Brien, is there a sister paper reporting anchorage loss or something equivalent? I think the two pieces of information (time and anchorage) should be considered together when making a decision on how to close space. If there is no difference in anchorage loss then the decision on how to treat is very easy.
You are not too critical of this study.Your valid comments are exactly why I read your blog avidly!
It’s a bit surprising, with some of the studies that you report on, what the level of initial problem is (such as overjet, often a bit small) or, in this case, the length of time for treatment. For the faster treatment the mean time to close a premolar space was apparently 13 months. I know these were adults but even so what was going on? In the 2 stage group this took 2 yrs!? And that’s just the space closure bit. This seems like particularly prolonged treatment, their patients must be very tolerant. Just saying.
I agree with the other comments, we need more information. Overall treatment time and whether treatment objectives were met, including anchorage loss, overjet and incisor proclination. Personally I use two stage when concerned about anchorage, usually until the canines are Class I, then it becomes en masse.
Thanks, Kevin:
I have two comments; #1. It looks like the 2-stage procedure took approx. twice as long. Not surprising – and this has nothing to do with ‘tooth movement’ per se. It may actually depend on the rate of bone remodeling, which doesn’t vary very much (unless it’s interfered with biochemically [bisphosphonates]). This means that in the 1-stage procedure, the treatment appeared faster since there was only one phase of bone remodeling. The 2-stage procedure took twice as long since there were ostensibly two phases of bone remodeling (both of which occurred at the same rate as the 1-stage procedure). In other words, there was no difference – both procedures were completed at the same rate.
#2 Why is it a ‘crime’ to extract premolars? Perhaps because it’s claimed that there are other unwanted side-effects. For example, a preliminary study (after correcting for size) indicated that premolar extractions may affect facial morphology, which may have subsequent effects in some cases.
Singh GD Maldonado L, Thind BS. Changes in the soft tissue facial profile following orthodontic extractions: a geometric morphometric study. Funct. Orthod. 22(1):34-40, 2005.
Excellent questions and review – patients WANT faster treatment and anything that can help is appreciated. Corporate exaggerations must be exposed and dental authority lawyers need to be educated to avoid torturing dental professionals with an interest in efficient treatment. Sad to report an orthodontist in Alberta is now being subject to an attack by the ‘Word Police’ who seem to believe quicker implies better and thus violates the ethical rules against claims of superiority. Amazing how lawyers with no formal training in dentistry are allowed to have such power over those who have dedicated their lives to this area of dentistry.
There have been several papers that evaluated anchorage loss with 2 step vs. en masse retraction
1. Heo et al PMID: 18004930- Retrospective study. Molars in both groups, moved mesially about 2 mm. No significant differences in the amount of anchorage loss.
2. Xu et. al PMID: 21055588 – RCT. Molars in both groups, moved mesially about 4.3 mm, with the 2-step group exhibiting slightly more anchorage loss. No significant differences in the amount of anchorage loss.
3. Schneider et al. PMID: 31259616 – RCT. Molars in both groups moved mesially about 3 mm. No significant differences in the amount of anchorage loss or incisor retraction, between the two groups
I can’t a find a reason for measuring the width of the premolar on the initial model. Their Kaplen-Meyer statistic does not need it and I didn’t find a mention of it in the results. Anybody have an idea why it was done?
Kevin,
One of the reasons that, in days gone by, canines were retracted first, where anterior crowding was the rational for bicuspid removal, was that no attachments were placed on the crowded anterior teeth until the there had been sufficient canine retraction to align the incisors without flaring. In today’s hurry up rational it is more common to place all of the attachments regardless of the arch length issues with full arch-wire engagement with resultant anterior and lateral flaring of the crowded teeth. Thus there is minimal decrease in the extraction site until retraction of the flared teeth begins. When incisors are flared to improve alignment labial crown torque is also increased.. Retraction of the flared segment, if accomplished on a an edgewise wire with no tipping, is going to require more anchorage than if the canines had been retracted first then incisors aligned without flaring or increase in labial crown torque. Point being that a flared anterior segment will require more time for distal space closure than one that is has not been flared, all other factors being the same, As in all clinical studies it is important to compare apples to apples..
Kevin,
One of the reasons that, in days gone by, canines were retracted first, where anterior crowding was the rational for bicuspid removal, was that no attachments were placed on the crowded anterior teeth until the there had been sufficient canine retraction to align the incisors without flaring. In today’s hurry up rational it is more common to place all of the attachments regardless of the arch length issues and full arch-wire engagement with resultant anterior and lateral flaring of the crowded teeth. Thus there is minimal decrease in the extraction site until retraction of the flared teeth begins. When incisors are flared to improve alignment labial crown torque is also increased.. Retraction of the flared segment, if accomplished on a an edgewise wire with no tipping, is going to require more anchorage than if the canines had been retracted first then incisors aligned without flaring or increase in labial crown torque. Point being that a flared anterior segment will require more time for distal space closure than one that is has not been flared, all other factors being the same, As in all clinical studies it is important to compare apples to apples..
2-step retraction has a different objective than en masse retraction. (Just look at their names!) Do you prefer apples or oranges?
Is there any difference regarding the loss of anchorage?