Three-dimensional CBCT imaging: Pretty pictures but a risk of cancer?
Very occasionally, I come across something in orthodontics that worries me. However, sometimes I also get cross. These CBCT images of a six-year-old do both.
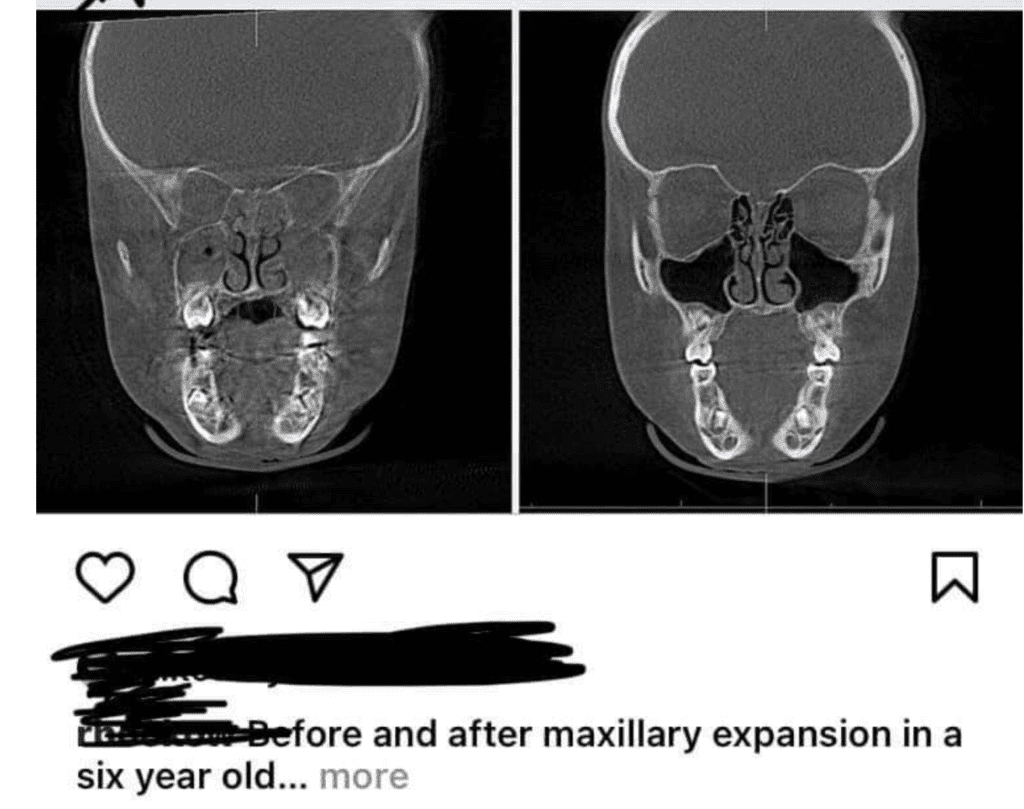
I was amazed when I saw this image on social media. An orthodontist or dentist posted it to illustrate the effect of maxillary expansion on a six-year-old. There are so many things wrong with this; I struggle to believe that this image is genuine. These are:
- Is there a need for imaging if we are treating the symptoms of a breathing disorder?
- The images are of different coronal sections, so they are valueless as an illustration.
- The operator has irradiated the child’s brain, and there is no need for this.
- There is no need for a post-expansion image. Either the treatment resolved the symptoms, or it did not? Sequential imaging is not needed.
- Did the parents and child properly consent to this radiation dose with doubtful benefit?
I wonder if this is an example of clinical negligence?
At the same time that I saw these images, a new paper on cancer risk from dental imaging was published. These are my thoughts on this new paper.
So let’s have a look at the paper, which was coincidentally published within a few days of the images that worried me so much.
The authors of this paper reported on the risk of cancer from dental radiographs. Two USA based investigators did the study. Oral Surgery, Oral Medicine, Oral Pathology and Oral Pathology published the paper. This is a highly respected journal.
Estimation of X-ray Radiation Related Cancers in U.S. Dental Offices: Is it worth the risk?
Douglas K. Benn , Peter S. Vig
Oral Surgery, Oral Medicine, Oral Pathology and Oral Pathology
I should start this blog with some information that we all should know, but I wonder if we have forgotten it? I extracted this useful information from the introduction to the paper.
We know that dental radiographs are low dose. As a result, a single radiograph is unlikely to cause harm. However, the risk from our imaging is stochastic and random. This effect may damage cells sufficiently to lead to cancer, possibly. Children are also more susceptible to the effects of ionising radiation. Furthermore, any head and neck cancer may be associated with diagnostic x-ray exposure. Nevertheless, we cannot prove any cause and effect. This is why we follow the ALARA guideline.
What did they ask?
They did this study to find information on primarily:
“The possible number of cancers produced during 2019 in U.S. Dental Offices from radiography”.
What did they do?
The authors used several sources of data to identify the following:
- Estimates for the number of dental radiography examinations in the USA.
- Estimates for the number of people undergoing a course of orthodontic treatment (From JCO surveys).
- The estimated rate of cancer incidence per million IO, Pan and Ceph radiographs and CBCT examinations.
- They also reviewed the frequency and nature of informed consent for radiographic examination.
I do not have the space to go into the details of the data sources or to review their validity here. The authors present a large amount of information in the paper.
What did they find?
I thought that their results were very worrying. Here are the main points:
- There were 300 million radiographic examinations. These may have resulted in 827 cancers, of which 114 were in children.
- For 5.1 million CBCT examinations, there were possibly 84 cancers, and 73% were in children.
When they looked at orthodontics:
- Twenty-one million patients started a course of treatment in 2020. The estimated total possible cancers were 135. They broke this down to: Full mouth examination 18, Pan 40, CBCT 71 and Ceph 6.
They also did some estimates for CBCT imaging as the use increases. Importantly, they built in the fact that as CBCT use increases, there will be a reduction in panoral and ceph images. They then calculated that CBCT examinations increased from 16% of ortho exams to 50% there would be an increase in cancers of 119 to a total of 254. If CBCT increased to 86%, CBCT cancers would increase to 343.
In their discussion, they pointed out that if a 10- to 14-year-old girl had 3 CBCTs over two years, the risk of her developing cancer was 1 in 6,000.
This scenario is particularly concerning when we consider that the JCO survey revealed that 16% of children attending orthodontic offices routinely had CBCT examinations.
Their overall conclusions were:
- Dentists are possibly causing 967 new cancers in the USA per year in the head and neck region.
- In 2020-21, all courses of orthodontic treatment may generate 135 cancers. A future increase in the use of CBCT images could cause 361 cancers, mostly in children.
What did I think?
This paper’s results and the social media posting of the six-year-old who had 2 CBCTs shocked me. I have looked at the document carefully. While the authors derive their data from readily available sources, they also make several large assumptions. As a result, we perhaps need to be cautious about their findings. Nevertheless, we are dealing with a serious issue, and I feel it is wise to be careful.
We also need to remember that many orthodontic studies suggest we do not need to use cephalometric radiographs for treatment planning. As yet, there is limited research done on the orthodontic diagnostic utility of CBCT. When these studies are done, I will wager that the results will be the same.
Radiographic guidelines also urge caution on the use of CBCT imaging, as this is a high dosage, and it may not be necessary.
Interestingly, the authors declared an interesting conflict of interest. They are both on the Clinical Advisory Board of Smile Direct Club. Does this make a difference to our interpretation?
Final thoughts
One of my jobs when I was training was in radiology. I learnt a lot from a very wise supervisor. He would often say “You should only take a radiograph if you are not reasonably certain of your diagnosis and plan”.
This is still true. Over many years we have been providing good orthodontic treatment without routine CBCT. Perhaps those who are taking CBCTs for routine patients need to improve their diagnosis and treatment planning, if the cost of their uncertainty is putting a child at unnecessary risk.
I cannot help thinking that we need to stop taking so many CBCT images for routine treatment. We don’t even need to consider whether we should be doing this to measure the dynamic airway and go down the quackery track.
I hope that all orthodontists read this paper and bear in mind its results the next time they want to take a pretty 3D picture of a child patient. Clearly, we need to ensure that we have sufficient information to hand to make informed treatment decisions. We also have a great responsibility for the health of our patients, and we should not abuse it.

Emeritus Professor of Orthodontics, University of Manchester, UK.
Taking a CBCT in these patients is totally wrong, european and national guidelines do not endorse this. This dentist could be suspended for doing this.
We are obliged to have our xray-machine checked, follow courses every 5 years, send in some xrays to have them checked by regulatory bodies every three years and there is an endless stream of bureaucratic legislation which changes almost continually to protect the general population. All this costs a lot of money.
Pretty much useless in the end if some idiot dentist or orthodontist just ignores simple basic principles like ALARA and irradiates his patients (and does not forget to charge them heftily without doubt) and gets away with it.
I really appreciate your review. It is food for thoughts.
I am glad to know own a CBCT
Kevin,
Thanks again for bringing things to the fore that might otherwise be swept under the rug. Lately I’ve begun to see one local ortho practice and several general dental offices pushing treating patients as young as four years old with expansion not for orthodontic purposes but instead purely for breathing. Speaking to the general dentists they can’t be swayed and if I won’t do it they will find an “enlightened” orthodontist who will.
Speaking of radiation exposure though, I wonder how many orthodontists continue to take cephalograms regularly when their diagnostic usefulness has been called into question as well.
It’s unfortunate that this post dwells so much on an individual, rather than radiographic risks. We were not in that clinician’s position. We don’t know what clinical findings were present which led the clinician to prescribe radiographs. Focusing on an individual, and making assumptions of their thoughts and intent, and suggesting censure and quackery are counterproductive. I’ve posted cases for colleagues to review, with serial radiographs. Fortunately for me, they were 2D, and not posted on a social-media marketing site.
In the United States, DIY Orthodontic companies such as SDC, have been blocked from doing business in a number of states. These state legislatures and or dental boards require an in an in person exam as well as radiographic exam prior to the start of any dental treatment. Wow, that kind of hurts the business model. More states are still reviewing or changing their dental regulations to address tele dentistry guidelines. As such the battle continues. Given the authors serious conflict of interest, I would not take their findings or conclusions too seriously. Looks like research designed to argue a cause.
Hi Kevin.
Excellent point. They will be trying to fill the literature with papers that support NOT taking pre-treatment xrays. As you said, that supports their business model.
Thank you for this post. Based on the concerns you noted, it seems these images were done for marketing purposes.
Your supervisor’s advice to only take an x-ray if you were unsure of the diagnosis is absolutely sound. Radiography should be an aid to diagnosis when and if required. However, your reference to linking breathing and quackery are unworthy and insulting; if you cannot see the importance of, and the connection between dentistry and breathing, you should be very worried.
This is an interesting study but the level of scaremongering is somewhat surprising. Dr O’Brien chose an emotive scan at the outset, which is not representative. First, the FoV is much larger than most orthodontists/dentists deploy. If indicated, we typically go from the cranial base down to the hyoid bone, avoiding unnecessary exposure to the brain. Next, the scan was presumably taken to monitor sinus health (not airway/breathing/sleep issues), and was possibly requested by an ENT/Radiologist (at least that has been our experience). Third, if we look at CBCT exposure in mSv, it’s about 10x less than an equivalent Medical CT scan. So do medical CTs cause 10x as many ‘cancers’? Fourth, what is an ‘orthodontic cancer’? I could not find one in the medical, dental or orthodontic literature. In any case, there appears to be a typo in the authors’ Conclusion. I believe it should say “Orthodontists are possibly causing 967 new cancers in the USA per year in the head and neck region” not “Dentists” since the data was based on orthodontic treatment. Interestingly, there are about 1.8M new cancer cases per year in the US, presumably unrelated to CBCT exposure. The way past these emotional concerns is to apply a robust measure of ALARA.
Disclaimer: I have no financial affiliations with any CBCT manufacturers/suppliers
We still use the lead apron for a panoramic view with the addition of the lead cervical shield (as well as the apron) for the lat ceph. This is despite the “authorities” saying we don’t need to with contemporary digital radiology. I happen to think that despite the low levels, every little bit helps. We cannot predict the future lifetime dose a patient may receive. Our patients and parents appreciate this additional protection, especially the parents of kids who are radiologists and oncologists!
The overuse of CBCT might be related to increased availability however the “business model” requires that the machine be paid for. I still prefer to have the Oral and Maxillofacial Surgeons arrange for CBCT views, as I think they interpret them with more expertise, given the nature of their training, the area they work in, and frequency / familiarity of use.
Great review. Some suggest that CBCT should be the standard for diagnosis and treatment planning. Interesting were your comments in regards to a Lat Ceph as well, great food for thought. good to see such a review.
One thing that is important to consider when reviewing these dose and cancer risk articles is that by their very nature they are based on the extrapolation of data embodied in what is called the “Linear no-threshold (LNT) theory” The evidence has been is mounting against this theory for a while. This article is research based on the assumption that a theory is true. Look up Linear no-threshold theory on pub-med. Do I feel that its a good idea to willy-nilly take x-rays on patients? No of course not. Do I think that x-rays should be used to “evaluate the airway”? Of course not, because the research suggests that x-rays are NOT a meaningful way of evaluating a persons ability to move air between their lungs and the environment. I have not read this paper, because I don’t have access, but most articles like this are all the same. The key point is, the science is evolving on low dose radiation and evidence is mounting against LNT. Moreover, the policies of large governing bodies are involved which makes everything more difficult and confusing. Things are changing however, slowly but surely. Seriously, look up linear no-threshold theory. For those of us that don’t want to read lots of pub med stuff, here is a good powerpoint that will save you many hours. https://www.slideshare.net/MohanDoss6/should-the-radiological-community-continue-the-present-radiation-dose-reduction-campaign-and-efforts-jrs-talk-4172015-revised-v103
Here is a good follow up presentation.
https://www.slideshare.net/MohanDoss6/xlntsari-aapm-2018-narrow-poster
I think we all need to think about the use of x-rays in orthodontics. How many lateral Cephs actually alter the treatment plan we had in our minds within 10 minutes of the patient walking in the door? How many people are taking lat Cephs during treatment to assess ‘incisor’ angles? I know of people that take them at the end of treatment as well, why I don’t really know ( for the vast majority of cases anyway). Is it just for medico-legal reasons to cover ourselves?
It’s an interesting question about the value of the Ceph, never mind CBCT. Back in the day there was a lot published about ceph tracing and working to certain values that appears to have gone. I still take cephs but never trace them since I am only interested in whether the teeth are proclined or retroclined or where the jaws are and am not interested in absolute values. Should I not be bothering even with that? I THINK that the ceph helps me to decide between extn and non extn or between surgery and compensating but maybe I’m deluding myself. Research needed, or is it out there somewhere and I haven’t read it?
https://www.facebook.com/seankcarlsondmdms.teacher/photos/a.980389542002675/5087333877974867
Thanks, so all this says to me is that there is still a risk from CBCT. The operator and the patients need to decide if this risk is acceptable. I certainly would not my grandchildren to have sequential unnecessary CBCTs.
Radiation safety as important as it is, you seem to be missing the point of the article. That we as dentists are responsible for helping children develop an optimal physiologic airway and breathing pattern is the point of the article. Deflecting the conversation away from the wonderful results that this orthodontist displayed should encourage you, not discourage you, from seeing this bigger role we can play in childrens’ overall health and wellbeing. For the naysayers in the crowd that are still ignoring our role in health, way beyond straight teeth and a pretty smile, consider this: Had the child in this paper been treated only for straight teeth, her chronic condition could have lingered for years unnoticed by her physician and parents and led to years of misery. Just ask the adults who now come to our offices begging for relief.
To be fair, not all breathing issues are due to dystrophic growth patterns and radiology is not the only data set that is needed to properly evaluate the airway. One must also look at the physiology of the airway for anything that creates constriction, obstruction, or collapse. One must also look at the habits, soft-tissue dysfunctions, and compensated breathing patterns (ie mouth breathing) that exacerbate hard tissue dystrophy. And certainly, not all of these are solved simply by a palatal expansion procedure alone.
But you’ll never be able to help children with these issues if you don’t see them….and especially if you refuse to look for them.
BTW, I do support ALARA principles and only take post-op CBCT’s when there is another reason to do so that will influence future treatment. That said, when evidence of success does show, it is certainly worth talking about.
Also, the ENTs that become part of my treatment team are amazed by what the CBCT reveals to them that endoscopy doesn’t show.
C’mon guys. Let’s get our heads out of the sand.
These articles shed light on a disturbing “dirty secret” that needs more critical thought and “sunlight” application.
Whilst some conclusions and extrapolations are a “little of a stretch”, the orthodontic profession needs to take a long, hard look at current radiographic precautions.
Dosages can be limited by:
A) good operation technique with minimal “re-takes”
B) using appropriate collimation
C) using fast receptors
D) minimizing imaging
The last point is critical and orthodontics needs to consider imaging based ALARA “as low as reasonably achievable” .
It is in my view thats we could work towards using 1 pan (only) at the initialization of therapy and only use additional when there are specific needs.
These authors have done us a great service.