A new study on pre-formed myofunctional appliances done in Syria provides interesting results.
Every now and then someone does a great study. A team in Syria did this study and publication has been delayed because of the Syrian Crisis. It is well worth a read.
This trial addressed the controversial treatment of myofunctional orthodontics. This treatment philosophy is based around early treatment with pre formed appliance and muscle exercises. A company based in Australia called Myofunctional Research make these appliances. Proponents claim that they are treating the cause of malocclusion and that the appliances are more effective than conventional treatment. Furthermore, the outcome of this treatment is more stable than conventional orthodontic care. In theory, this has some logic. However, despite widespread promotion by Myofunctional Research, evidence regarding these claims is lacking. I have posted about this before and had an interesting discussion with the scientific advisor to Myofunctional Research. Initially, they appeared interested in carrying out some research with me as an advisor, but when I asked him if he was prepared to do a study in which patients were randomised to conventional and myofunctional treatment, the silence was deafening.
A team in Syria did this study. It is an example to all those who resist carrying out trials into their products.
Ghassan Idris et al
European Journal of Orthodontics, 2018, 1–8 doi:10.1093/ejo/cjy014
They asked;
“What are the soft and hard tissue effects of an activator and a pre formed myofunctional appliance”?
What did they do?
The PICO was;
Participants: 8-12 year old children with overjets greater than 4mm. They recruited the patients via a screening programme.
Intervention: Myofunctional Trainer for Kids (T4K). This is a pre-formed appliance. The children were asked to wear this for two hours a day and when sleeping. All participants had soft trainers for the first 6 months, then hard trainers were used for the remaining period of the treatment. They also did a series of daily muscular and swallowing exercises.
Comparator: Conventional activator worn for 15 hours a day
Outcome: Cephalometric analysis at the start of treatment and 12 months later.
They carried out a good sample size calculation. They based this on a difference in ANB of one degree. This is rather small and I wondered if the study was over powered. However, it showed that they needed 30 participants in each group. This reduced the problem of a small study reporting spurious effects.
They used a pre-determined randomisation and concealed their allocation with sealed envelopes. Unfortunately, it was not clear whether patient enrollment was done before the allocation. This does put the trial at some risk of bias.
What did they find?
They randomised 30 patients to each of the interventions. At the end of the study, 2 of the activator and 4 of the T4K groups dropped out.
They presented a large amount of cephalometric data and this was a little confusing. As a result, I have just selected some of the most important final treatment outcome measures in this table.
| Final outcome | Activator | T4K | p |
| ANB | 4.53 (1.69) | 6.21 (2.04) | 0.001 |
| Wits | 1.57 (1.44) | 2.50 (1.69) | 0.2 |
| Overjet | 4.20 (2.1) | 4.61 (2.14) | 0.001 |
They concluded that a 12 month treatment with an activator resulted in better skeletal change than the T4K. Furthermore, the activator was also better than the T4K in reducing the overjet and normalising the soft tissue pattern.
In their discussion, they suggested that this may have occurred because of the greater wear time of the activator. They also pointed out that the T4K was rather flexible and did not hold the mandible forwards as much as the activator.
What did I think?
I thought that this was a well carried out interesting study. The good points were:
- They investigated a clinically relevant question
- The trial had an adequate number of patients and there were few drop outs.
- Randomisation and concealment were good.
- They recorded and analysed the data blind.
These issues were potentially problematic;
- It was not clear whether they allocated the treatment after they enrolled the patients into the trial. This means that there is potential for bias. Nevertheless, the groups were similar at baseline.
- They only measured cephalometric data. Furthermore, the differences between the two groups after treatment were rather small. I did not feel that they were clinically significant.
If we put all this together. I feel that this papers provides us with useful clinical information and suggests that the there are no real clinical differences between activator and T4K treatment.
We now need to consider whether there is an advantage of the T4K because it is pre-formed and can be fitted without impressions. I think that this is a considerable benefit of this type of appliance. I would also like to see further research on the end of treatment results with this appliance.
Final comments
Finally, I would like to consider whether the results of this study and an earlier study by Emina Circic support the advertising claims made by Myofunctional Research. I have looked at their website and they make claims about improving breathing, arch development, better jaw growth and long term stability of their treatment. This study does not support their claims. Perhaps they should do some research into these claims before they make them. After all a team from Syria has managed to research into their product….
However, it does appear that the myofunctional appliances that have been tested in the two trials produce similar results to conventional activators. This could be a great selling point to orthodontists. There would be no need to promote their appliances by making reference to magic claims. I wonder why they don’t do this?
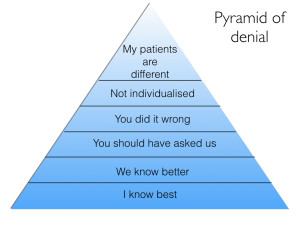
Let’s have a good discussion, but before you make a comment, please remember the pyramid of denial..

Emeritus Professor of Orthodontics, University of Manchester, UK.
 Soft- and hard-tissue changes following treatment of Class II division 1 malocclusion with Activator versus Trainer: a randomized controlled trial
Soft- and hard-tissue changes following treatment of Class II division 1 malocclusion with Activator versus Trainer: a randomized controlled trial
Impressive work by the team from Syria. Probably, for the first time we have some reliable data on myofunctional trainers. As mentioned by Dr. O’Brien further research is required to ascertain whether they hold an actual edge as far as clinical results go.
Interesting paper. Kevin do you think it would have been even more interesting if they had a third “no treatment” group?
Yes, it would. a possible design would be similar to the classic early class II studies. I thought that their data was similar to the functional appliance arm of these studies. However, their study was designed to compare the difference between the two treatments and not a control.
Morning,
This is a great study testing a new form of brace and showing that it’s essentially doing the same as the old brace. I think we can now assume that anything that holds the jaw open and forwards a bit will do the same thing. My only initial thought was that over 4mm of OJ could possibly be not much OJ at all and maybe they were intercepting something that may have just self-corrected with growth.
It strikes me that quite a few early functional cases get retreated later with extns so could possibly be a waste of time and in the urge to always be doing something we are inflicting needless braces on people. Could the most effective way to treat Class 2 be wait until growth spurt is over (like you do for class 3) and then camouflage with extns, if necessary, or do surgery or accept a class 2. Can we ditch the functional altogether? It would be interesting to compare different methods of treating class 2 from round the world and look at the end results to see if you could tell the difference.
I still use a functional type brace now and again but am starting to lose the faith.
Dear Kevin
As you mentioned, ‘they only measured cephalometric data’ and that the differences were likely not significant.
Two observervations:
1. If some (maybe all?) of the children from this trial had pre-Tx skeletal CL II malocclusion (excess OJ/large ANB difference) by age 8, at what age do you think this particular malocclusion phenotype might have been first detectable in some (all?) of these kids ? And;
2. Do you think that maybe adding validated questions (e.g., Chervin Pediatric Sleep Questionnaire, B.E.A.R.S., etc.) about sleep and airway hygiene as inclusion criteria might have made thus study protocol more robust and useful?
2.
Thanks, in answer to your questions. It is not possible to say with any real certainty on when the malocclusions became evident, but my clinical experience would tell me that most were evident at about 5-6 years old.
Yes, it would have been great to use other outcome measures, particularly those that are concerned with breathing etc. However, this small study is a great first step and I would like to see more with other outcomes. Perhaps, myofunctional research will run some?
Dear Kevin
To your statement, ‘It is not possible to say with any real certainty on when the malocclusions became evident, but my clinical experience would tell me that most were evident at about 5-6 years old.’ I don’t think you’d get a sound and scientifically-supported argument from anybody regarding your experienced opinion that most Class II phenotypes here were evident but 5-6 years old. But, I do think your stated opinion that ‘it is not possible to say with any real certainty on when the malocclusions became evident’ is not very well supported. In 2005 Antonini published a well referenced paper in Angle Orthd.(75(6):980.) that referenced several articles regarding when class II phenotypes are first detectable:
Excerpt:
Early traits of a Class II malocclusion are observable in the deciduous dentition.1–10 Foster and Hamilton3 studied British children from 2.5 to three years and reported a 38.8% prevalence of distal step of the second deciduous molars and a 59% prevalence of Class II deciduous canine relationships. The respective values in Finnish children were reported to be 43.3% and 68.1%.4 Bishara et al reported that a full Class II malocclusion in the deciduous dentition is never self-correcting in growing children.5 Several reports have noted that a distal-step relationship of the second deciduous molars leads to a Class II relationship of the first permanent molars in the transition from the deciduous to the mixed dentition.5–10
Additionally, I can give you several references of papers that had been published in peer-reviewed medical and dental journals dating back from the mid-19th thru early to mid-20th Centuries that support, not only, that so-called (by EH ANGLE et al) ‘Disto-occlusion’ (i.e.,Class II skeletal) as being readily detectable in the primary dentition, but always persists and worsen beyond…..And, as Class II is often co-morbid with naso-respiratory incompetence/habitual mouth-breathing, near-behavioral/neuro-cognative deficits, should be intervened upon at the soonest possible opportunity.
Granted Kevin, that these afore-mentioned papers were not reporting on prospective, double-blinded, longitudinal RCT’s, but prospective, blinded RCT’s would be impossible to perform within this framework given what IRB committees ethically require (since the trials at Nuremberg from where our current IRB system first arose) from protocol proposals/inclusion criteria in terms of withholding a potentially beneficial treatment modality (e.g., class II correction in the primary dentition) from a control cohort.
Your blog generates much discussion on some very important issues Kevin and I am pleased to see it growing in popularity. I am hopeful, however, that discussions will continue to gradually move more and more towards the topic of optimizing development of the inseparable ‘craniofacial and respiratory complexes, and at earlier stages in a child’s somatic and neurologic development than is now current practice.
Can these results be extrapolated to compare against a twin block?
I would like to add that an argument could be that this type of clinical approach (using a consecutive set of “trainers”) should have been started earlier (3-4 years olds) as per suggestions by the company marketing. So this specific study answers if there are cephalometric differences when started in mid or late mixed dentition. Again just a small piece of information from a big puzzle. What would be really interesting is to assess the oral function improvements that are claimed to occur. Sadly those are difficult to assess with current technology. So until possible is a question that stays in the air.
Also the patient relevant question is if let’s say 8 years of continuous treatment compared to 2-3 years of “conventional” approach is clinically meaningful for the patient perception and oral functions. Biological, financial and compliance costs have all to be taken into account before having a strong answer.
Thanks for this
As I understand it, certain skeletal patterns respond better to functional appliances- is this accounted for when selecting patients for intervention and control groups in studies like these?
Stephen Murray
Swords Orthodontics
So in summary regarding Class II correction we have;
1) The Activator = Fxn Appliance for Class II correction (+ passive arch expansion from buccal shields)
2) T4K is similar if not slightly inferior to Activator in Tx result, but is more convenient and possibly a lot cheaper to implement… if we want to do 2-phased Tx (which is more expensive than Single-phase).
However, we shouldn’t forget;
3) 2-phase Tx in Class II cases generally produces the same outcome as Single-phase Tx
… which is the cheapest Tx option
Unless we choose to observe growth and hope for spontaneous resolution that is unlikely.
Dear Ben
Has there ever been any published evidence to support that so-called ‘spontaneous resolution’ of a class II malocclusion phenotype, can/does occur? You indicate that it ‘is unlikely’, which could be interpreted that it is still maybe possible?
Differential growth of the mandible has been demonstrated, and Proffit has written about the transition from primary molar ‘mesial step’ occlusion into the ‘Class I molar’ permanent dentition without definitive statements that what you see is what you get (although this is confounded by dental movement, and includes differential jaw growth.)
I suppose I subscribe to the notion that some people will have more differential growth than others (albeit, this assumes a deviation from their growth pattern), but these cases are not the majority.
Did I perhaps miss something here?
it is nice to praise research
A larger start ANB might be comparable to the “average ” case we ,as Orthodontists,treat with functional appliances and show greater, more valuable changes .
I like the prospect of relatively cheap, simple, impression free , part time ,more retentive, eruption guidance ,appliance,which can also be used a s a sports guard.More comparative wear time- homework, Tv ,travelling,sports and night time wear -should bring this up to matching the activator wear time.
The prospect of real overate reduction ,with simple ,non invasive treatment is to be commended ,applauded and encouraged .
I look forward t a study with better fitting appliances, more likely to produce desired changes